AAE Discussion Open Forum
Dear AAE,
I am Naoto Yoshida, an Active Member certified by the Association of Active Experts (AAE) since 1983. I have previously made a post titled "Memory with the great professor Grossman" on AAE's official website. Currently, I am active on the Japanese platform "note" since the onset of the COVID-19 pandemic, and my posts have attracted approximately 23,000 visitors. Most of the visitors to my note site are professionals in the medical field, including dentists.
I am interested in featuring information about AAE on my note site to widely introduce AAE's daily activities to the Japanese audience. Specifically, I would like to use parts of AAE's logo and website content.
I kindly request official permission from AAE regarding this matter. Through my website, I aim to spread awareness about AAE's valuable initiatives within Japan, contributing to the clinical practices of Japanese dentists. I sincerely hope for your favorable consideration.
Best regards,
Naoto Yoshida AAE Certified Active Member
--------------------------------------------------------------------------------------
**********************************************************************************
--------------------------------------------------------------------------------------
AAE Discussion Open Forum
Post New Message Feb 15, 2024 Discussions
started 3 days ago, Douglas N. Robertson (14 replies) how would you proceed here? 1. Brent, It may just add confusion if we don... Douglas N. Robertson 2. Patients who presented with a bad taste and odor... Harvey E. Matheny 3. Thanks Harvey, I'll check that tomorrow as well.... Douglas N. Robertson started 3 years ago, Keith V. Krell (12 replies) Introduce Yourself 4. Hello all, I am a new member of AAE and... Ameer Ahmed

top next 1. Re: how would you proceed here? Reply via Email Direct Reply to Sender Feb 15, 2024 7:33 AM Douglas N. Robertson Brent,
It may just add confusion if we don't know how to handle the additional information. But if you go back and read my post carefully, you'll see that an EPT result is not going to make or break the diagnostic threshold for me. It may make or break the decision to plan a recall or to not bother.
And that there's the debate of "muddying the waters" vs my "additional information is not a problem - it's what we may ill-advisedly do with that additional information" in a nutshell.
Doug
------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-14-2024 05:11 PM
From: Brent M. Hiebert
Subject: how would you proceed here?
I'm curious what @Richard S. Schwartz thinks of EPT testing....
For me, EPT would not convince me one way or the other for treatment. It will just add confusion. I'll stick to my original suggestion of monitoring and re-evaluate in 3-6 months with updated imaging.
I'll be interested to see what you find.
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures
top previous next 2. Re: how would you proceed here? Reply via Email Direct Reply to Sender Feb 15, 2024 9:10 AM Harvey E. Matheny Patients who presented with a bad taste and odor in spite of careful hygiene and use of flavored rinses often had a loose bridge retainer. Sometimes my office was just the last stop of many to their GP, a friend’s GP, and a periodontist.
Although this bridge is relatively new, I would check it anyway. Dry the area with gauze, isolate with cotton rolls, lift each retainer with an explorer or curette, and press back down while looking for bubbles at the margins through your microscope. Worth a try.
Sent from my iPhone
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 2/12/2024 11:01:00 AM
From: Douglas N. Robertson
Subject: how would you proceed here?
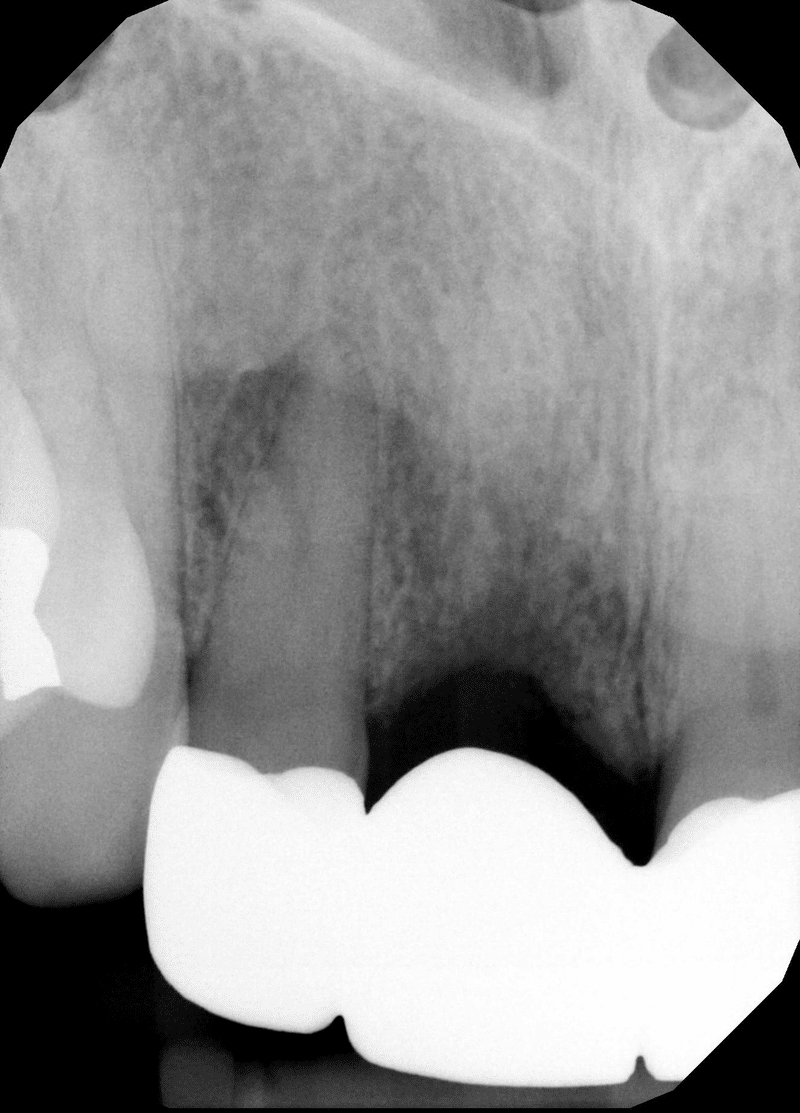
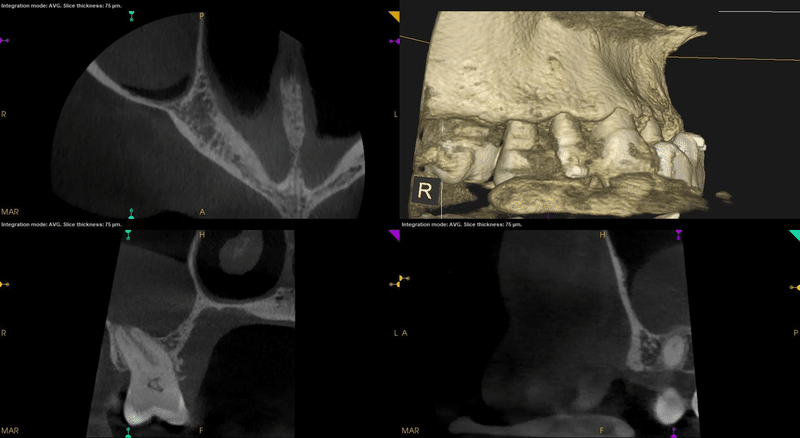
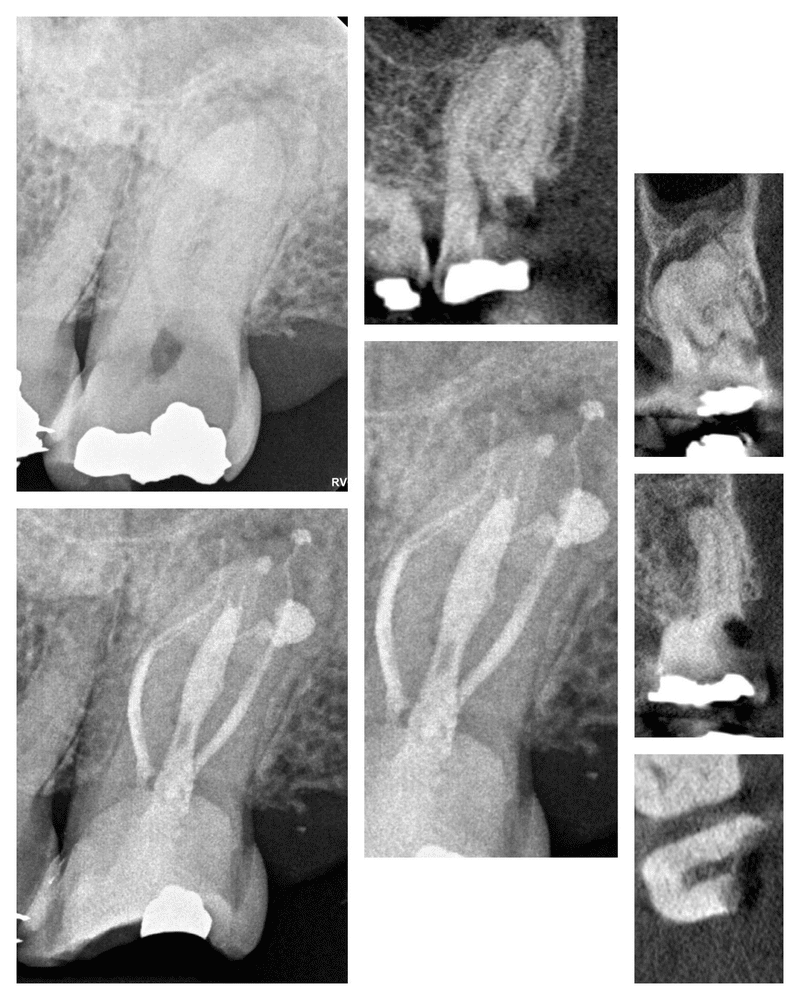
This patient in for a consultation last week. 64yoF had #8 extracted and the bridge placed about a year ago. She suspects either her sinus or #7 is responsible for drainage and a bad taste. #6 was slightly tender to percussion, and #6 -7 B mucosa tender to palpation. There was no obvious swelling or inflammation noted. #6 and #9 responded to cold test while #7 did not. I figured #7 must be a chronic abscess, but the surrounding bone looks perfect on the CBCT. Granted, there may be a slight fenestration near the apex, but it appears the main canal exits in bone.
Metal Artifact Reduction was applied for the CBCT.
The PAX that was sent to us has a relative radiolucency over #7 -8 area, but this appears to be artifact for #7 as I was unable to reproduce it on CBCT with 12mm thickness reconstruction. CBCT confirms #7 has no obvious defects or large lateral canals.
We also noted on the CBCT a R mx sinus mucocele. It's a common finding, and located posterior to the #7 patient-identified suspect, but I wonder if the symptoms could be related. The #8 extraction site also seems quite deficient in bony healing, but this appears to be unrelated to the chief complaint as there was no palpation tenderness here.
I wish I could do an electric pulp test for #7 . Unconvincing signs and symptoms, including the lack of cold response where the coronal aspect appears calcified, seems to be weak overall evidence for just doing a RCT. Would anyone do a pulp test cavity in this scenario? Or any other ideas on how to proceed?
Thanks,
Doug



------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV
------------------------------

top previous next 3. Re: how would you proceed here? Reply via Email Direct Reply to Sender Feb 15, 2024 9:36 AM Douglas N. Robertson Thanks Harvey, I'll check that tomorrow as well. Also planning to do cold test for the UR posterior teeth, just under that mucocele, though #3 is captured in the scan and there appears to be no relationship.
------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-15-2024 09:10 AM
From: Harvey E. Matheny
Subject: how would you proceed here?
Patients who presented with a bad taste and odor in spite of careful hygiene and use of flavored rinses often had a loose bridge retainer. Sometimes my office was just the last stop of many to their GP, a friend's GP, and a periodontist.
Although this bridge is relatively new, I would check it anyway. Dry the area with gauze, isolate with cotton rolls, lift each retainer with an explorer or curette, and press back down while looking for bubbles at the margins through your microscope. Worth a try.
Sent from my iPhone
Original Message:
Sent: 2/12/2024 11:01:00 AM
From: Douglas N. Robertson
Subject: how would you proceed here?
This patient in for a consultation last week. 64yoF had #8 extracted and the bridge placed about a year ago. She suspects either her sinus or #7 is responsible for drainage and a bad taste. #6 was slightly tender to percussion, and #6 -7 B mucosa tender to palpation. There was no obvious swelling or inflammation noted. #6 and #9 responded to cold test while #7 did not. I figured #7 must be a chronic abscess, but the surrounding bone looks perfect on the CBCT. Granted, there may be a slight fenestration near the apex, but it appears the main canal exits in bone.
Metal Artifact Reduction was applied for the CBCT.
The PAX that was sent to us has a relative radiolucency over #7 -8 area, but this appears to be artifact for #7 as I was unable to reproduce it on CBCT with 12mm thickness reconstruction. CBCT confirms #7 has no obvious defects or large lateral canals.
We also noted on the CBCT a R mx sinus mucocele. It's a common finding, and located posterior to the #7 patient-identified suspect, but I wonder if the symptoms could be related. The #8 extraction site also seems quite deficient in bony healing, but this appears to be unrelated to the chief complaint as there was no palpation tenderness here.
I wish I could do an electric pulp test for #7 . Unconvincing signs and symptoms, including the lack of cold response where the coronal aspect appears calcified, seems to be weak overall evidence for just doing a RCT. Would anyone do a pulp test cavity in this scenario? Or any other ideas on how to proceed?
Thanks,
Doug

------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV
------------------------------

top previous 4. Re: Introduce Yourself Reply via Email Direct Reply to Sender Feb 15, 2024 1:01 PM Ameer Ahmed Hello all,
I am a new member of AAE and very excited to be part of the community! I am a third year dental student at Boston University, where I also completed an MS in Oral Health Sciences and a BA in biology (you might be able to tell that I'm a Massachusetts native ;) )
I am planning on applying to a GPR this year in order to help myself better understand all of the disciplines in dentistry. While I plan on applying to Endo Residency next year, I first desire more experience in other disciplines as I feel that will help me understand each patient better. Looking forward to connecting with others here and hearing any guidance others have to offer! Thank you!
------------------------------
Ameer Ahmed M.S.
Boston MA
ahahmed@bu.edu
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 06-09-2020 08:37 AM
From: Keith V. Krell
Subject: Introduce Yourself
One of the perks of the AAE Discussion Open Forum is having the opportunity to connect with professional peers virtually. Use this thread to say hello and introduce yourself to the community.
Not sure what to share? Consider these questions:
What are your current or former roles?
Where are you located?
Why do you love endodontics?
What is something interesting about you that others may not know?
To kick off the introductions, here are a few facts about me:
I am from Houston, but have lived in Iowa for 45 years. In addition to being the past president of AAE, I have been the past president of the Foundation, past president of the ABE, and an Adjunct Clinical Professor at the University of Iowa.
I have been an endodontist since 1981 and enjoy the gratification of taking a patient from an extremely painful starting point to being pain-free. The technical intricacies are challenging and humbling but again having someone "thank you" at the end of an appointment is rewarding in itself.
A fun fact is that I have played the guitar since 1958 and have collect guitars for 30 years!
I am looking forward to meeting you! Reply now and share your introduction.
------------------------------
Keith Krell D.D.S.,M.S.,M.A.
Past President AAE, ABE, AAEF
------------------------------
-----------------------------------------------------------
----------------------------------------------------------------
Post New Message Feb 16, 2024 Discussions

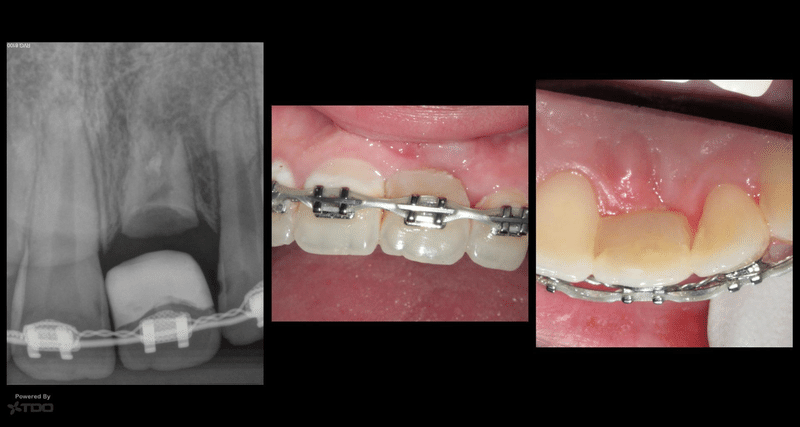
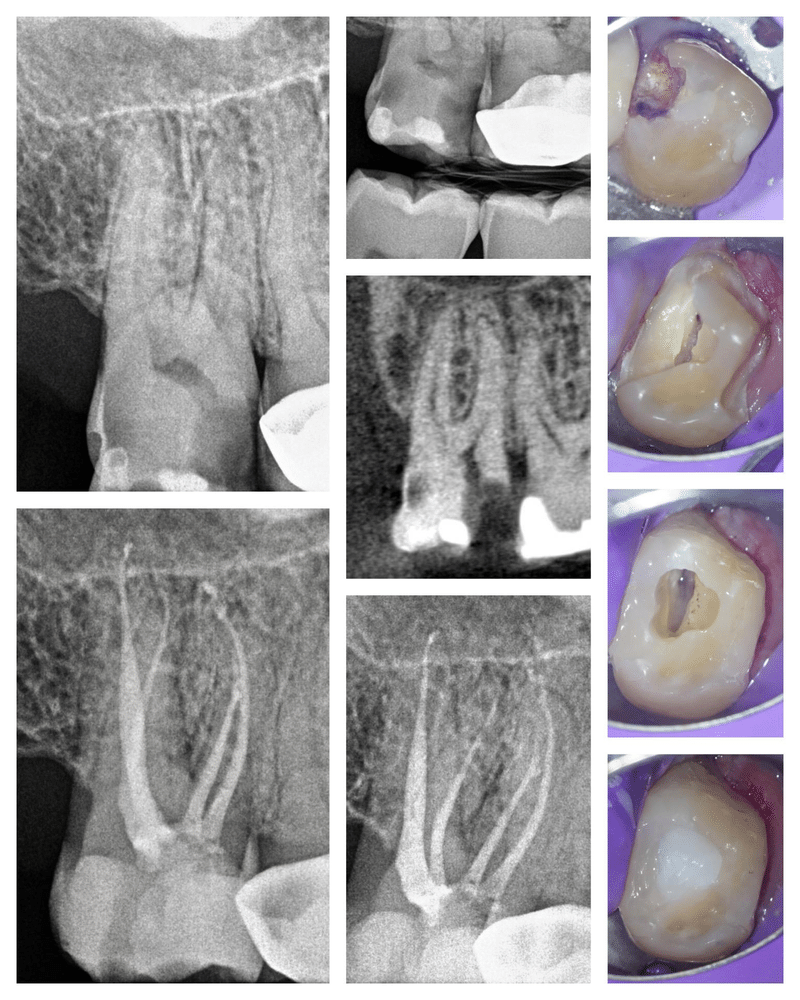
top next 1. Retreat of RCT done on Immature Roots Reply via Email Direct Reply to Sender Feb 16, 2024 6:30 PM Cami E. Ferris-Wong Curious how others would approach this case:
21 y.o. male traveled over an hour to come get a second opinion (actually fourth opinion, but I digress). Had RCT #15 done when he was 14 y.o. At the time the roots were not completely formed and he thinks they did it in one visit. He was told to get the crown when he was older. Had the crown done last July and then last weekend had swelling and pain (worst he'd ever felt, couldn't even open his mouth). His dentist prescribed an antibiotic and things calmed down, asympto today to perc palp and chewing. Tooth #14 tested WNL to cold. This week he got three differing opinions from two different dentists and an endodontist this week.


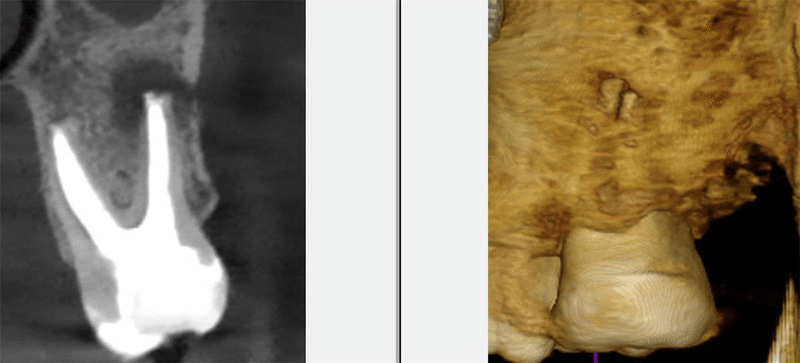
One thought the lesion was coming from #14 and wanted to do RCT on #14 (thankfully this was not the endodontist that said this). One said there was a root fracture and the tooth should be removed. One said the lesion was large and so the tooth should be removed. What say you?
Smiles,
Cami
P.S. I'll tell you what I said later.
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate
top previous next 2. SCAM ALERT: Safeguard Your Practice Against Fraud Attempts Linked to the Corporate Transparency Act Reply via Email Direct Reply to Sender Feb 16, 2024 4:54 PM Darcy McLaughlin AAE Members,
The Corporate Transparency Act, a new law, mandates businesses with fewer than 20 employees or generating less than $5 million in annual revenue to file a business ownership report with FinCEN before the January 1, 2025, deadline. Regrettably, this law is a new opportunity for scammers to pose as government agencies to steal money and personal information. We strongly advise our members to use only the official FinCEN website for filing reports and contact the agency directly with any inquiries.
You can learn more about the Corporate Transparency Act and what its reporting requirements mean for dental practices on our webpage here.
To protect your business from scams, consider the following tips:
Always verify with government agencies: Federal government agencies will never initiate contact via calls, emails, texts, or social media messages for payment or personal information. If you receive a letter from a government agency, such as FinCen, that requests money or personal information, you should always verify its authenticity directly with the agency.
Visit USA.gov to ensure the agency is real and that the contact information is correct. We recommend that you call the federal agency directly from the contact information listed on their government website to verify a letter. You should not use the contact information listed on the potential scam communication as it is likely fraudulent.
Finally, we encourage members to educate their office staff regularly on fraud prevention to protect your business. The FTC provides free brochures and resources to facilitate ongoing education efforts.
------------------------------
Darcy McLaughlin
Advocacy Manager
AAE
Chicago IL
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate

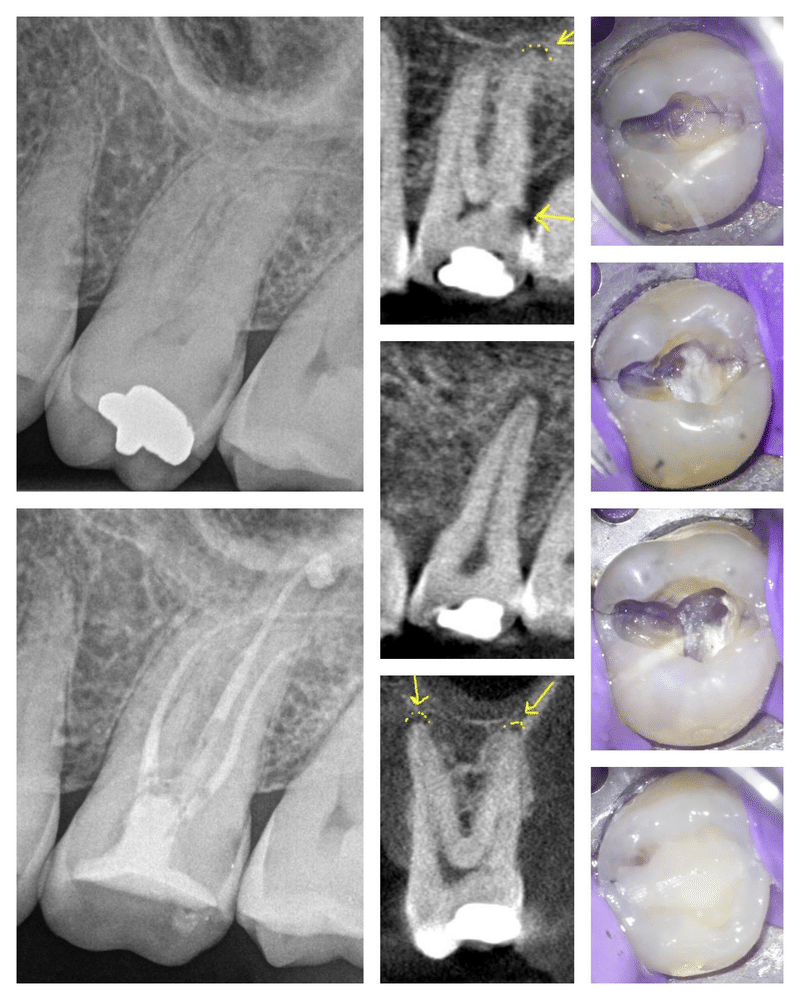
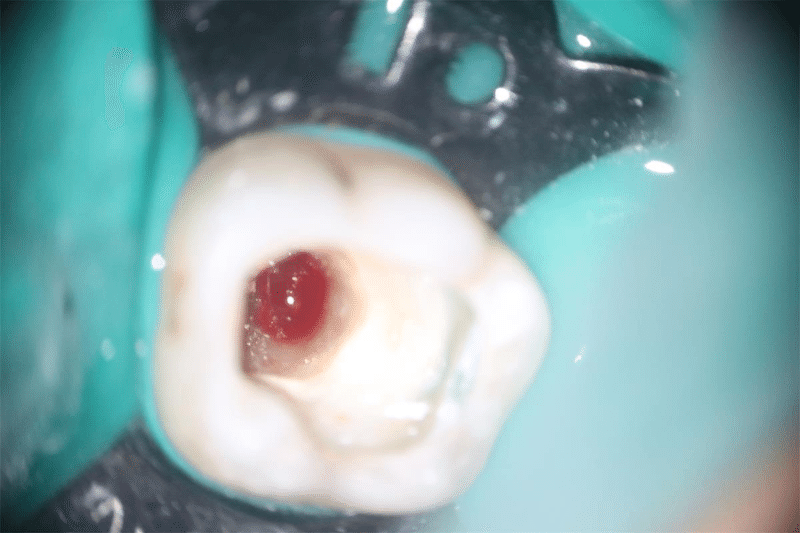
top previous next 3. Restorative Endodontics - Two cases Reply via Email Direct Reply to Sender Feb 16, 2024 8:02 AM Brent M. Hiebert Case 1: Tooth 15. An emotionally traumatizing Endo-restorative case. Lots of laser-ing. 23mm roots with curvature. The middle and apical 1/3 of the palatal canal was filled with pulp stones/calcifications and proved difficult to remove - not sure I even got all of it out. The DB buccal caries was extensive and required a rebuild to properly irrigate and run my laser.



------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate

top previous next 4. Re: how would you proceed here? Reply via Email Direct Reply to Sender Feb 16, 2024 7:37 AM Brent M. Hiebert Doug,
There is certainly no harm in collecting the additional EPT information. My comment was not meant to discourage your fact finding. I'm just keeping the conversation going. You'll have keep us posted on what you uncover during your next exploration of the patient's mouth.
Brent
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-15-2024 07:32 AM
From: Douglas N. Robertson
Subject: how would you proceed here?
Brent,
It may just add confusion if we don't know how to handle the additional information. But if you go back and read my post carefully, you'll see that an EPT result is not going to make or break the diagnostic threshold for me. It may make or break the decision to plan a recall or to not bother.
And that there's the debate of "muddying the waters" vs my "additional information is not a problem - it's what we may ill-advisedly do with that additional information" in a nutshell.
Doug
------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV
top previous next 5. Re: how would you proceed here? Reply via Email Direct Reply to Sender Feb 16, 2024 9:58 AM Steven P. Delgado Kudos Brent. Interesting learning case for residents etc. In my humble opinion, neither cold nor ept is indicated in this case from the beginning. The initial "tests" for me would be as you and others have described--patient education, checking for loose bridge, possibly hygiene improvements, and active monitoring at 3 months and possibly 6 months with updated imaging as needed. In general in medicine and dentistry (not talking about anyone or any case specifically), over testing often leads to over diagnosis leads to over treatment leads to faster tooth morbidity and tooth mortality. :-) Hopefully nobody is offended by that--that's just what is well established in the medical field for the last 50 or so years.
Just 2 cents to the discussion for residents etc. Happy weekend to all.
sd
------------------------------
Steve Delgado
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-14-2024 05:11 PM
From: Brent M. Hiebert
Subject: how would you proceed here?
I'm curious what @Richard S. Schwartz thinks of EPT testing....
For me, EPT would not convince me one way or the other for treatment. It will just add confusion. I'll stick to my original suggestion of monitoring and re-evaluate in 3-6 months with updated imaging.
I'll be interested to see what you find.
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures

top previous next 6. Re: how would you proceed here? Reply via Email Direct Reply to Sender Feb 16, 2024 3:47 PM Douglas N. Robertson There was no evidence of the bridge being loose when I checked it today. The patient felt the electric test more in the gums than in the tooth for #7 , and possibly for #9 , while for #10 (not part of FPD), she definitely felt it in the tooth. She mentioned she's never had a RCT, so I couldn't compare this sensation to a pulpless tooth. Clinically, I checked #2 -5 this time; #2 -4 responded to cold, while #5 did not. #5 has a DO-A a with a crack at the M which appears significant on transillumination. #2 -5 were WNL to percussion and palpation; and #5 was negative to ToothSlooth, with probe depths WNL without bleeding. I mentioned the option of a crown for #5 if she would wish to be more proactive in protecting against crown propagation.
Even with clearer EPT results, and had they indicated a lack of response, I would not have leaned towards RCT because the patient's chief complaint and other findings don't align with such a decision. It's challenging to justify RCT here when the bone looks completely normal around the apex.
I agree it's a potentially good learning case, especially for those who might not yet discern when to sideline findings with limited diagnostic value in certain contexts. Collecting baseline data at a patient's initial visit isn't something I'd discourage.
------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-15-2024 09:35 AM
From: Douglas N. Robertson
Subject: how would you proceed here?
Thanks Harvey, I'll check that tomorrow as well. Also planning to do cold test for the UR posterior teeth, just under that mucocele, though #3 is captured in the scan and there appears to be no relationship.
------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV

top previous next 7. Re: Introduce Yourself Reply via Email Direct Reply to Sender Feb 16, 2024 11:31 AM Tung B. Bui Good morning and happy Friday!
Thank you Ameer, for introducing yourself. Your initiative to participate in the Introduce Yourself thread is greatly appreciated. It's wonderful to see the community growing and becoming more active.
Your contributions and perspectives are valuable additions to our community, and we look forward to getting to know you better.
Once again, thank you Ameer, for your spirit and dedication to fostering a supportive environment within our association.
Cheers!
------------------------------
Tung Bui, DDS, FICD
Diplomate ABE
Southern Arizona Endodontics
Tucson AZ
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-15-2024 01:00 PM
From: Ameer Ahmed
Subject: Introduce Yourself
Hello all,
I am a new member of AAE and very excited to be part of the community! I am a third year dental student at Boston University, where I also completed an MS in Oral Health Sciences and a BA in biology (you might be able to tell that I'm a Massachusetts native ;) )
I am planning on applying to a GPR this year in order to help myself better understand all of the disciplines in dentistry. While I plan on applying to Endo Residency next year, I first desire more experience in other disciplines as I feel that will help me understand each patient better. Looking forward to connecting with others here and hearing any guidance others have to offer! Thank you!
------------------------------
Ameer Ahmed M.S.
Boston MA
ahahmed@bu.edu

top previous 8. Re: Introduce Yourself Reply via Email Direct Reply to Sender Feb 16, 2024 6:04 PM Cami E. Ferris-Wong Hi Ameer, and welcome from a fellow BU Alum (Endo '00).
I somehow missed this thread when Keith introduced it back in 2020 and glad to see it revived here.
I started posting cases a couple of years ago and try to do so whenever I get something interesting, though often times life gets in the way so I have a list of several cases to post but just haven't got around to it. Those who have read my posts over the years know that I feel strongly about a few things: Endodontists should do endodontic surgery, should be permanently restoring teeth and should consider taking a CBCT for every case, as it is unbelievable the amount of information we get even on "easy" cases.
I am a Diplomate of the Board of Endo, have practiced in Santa Barbara, CA for the past 24 years, have been involved with local study clubs over the years and go every year to the BU Endo Alumni meeting and AAE which keeps me up to date on the latest endo techniques.
I am married to an endodontist who practices north of here, in Lompoc (home of Vandenberg Space Force Base). We talk shop more than we should around the dinner table, but none of our three daughters have caught the bug. They mostly want to do anything except be a dentist.
I love beach volleyball and play almost every weekend. (You can still do that even during what is considered a rainy year for Santa Barbara).
Hope to see more people posting!
Smiles,
Cami
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-15-2024 01:00 PM
From: Ameer Ahmed
Subject: Introduce Yourself
Hello all,
I am a new member of AAE and very excited to be part of the community! I am a third year dental student at Boston University, where I also completed an MS in Oral Health Sciences and a BA in biology (you might be able to tell that I'm a Massachusetts native ;) )
I am planning on applying to a GPR this year in order to help myself better understand all of the disciplines in dentistry. While I plan on applying to Endo Residency next year, I first desire more experience in other disciplines as I feel that will help me understand each patient better. Looking forward to connecting with others here and hearing any guidance others have to offer! Thank you!
------------------------------
Ameer Ahmed M.S.
Boston MA
ahahmed@bu.edu
------------------------------------------------------------------------------
-------------------------------------------------------------------------------
Post New Message Feb 4, 2024 Discussions
started 22 hours ago, Brent M. Hiebert (0 replies) Cracked tooth. Ribbond used in the chamber. 1. Following amalgam removal and access, I noted... Brent M. Hiebert started 22 hours ago, Brent M. Hiebert (0 replies) C-Shaped Canal. 2.5yr followup 2. The patient returned for treatment of a... Brent M. Hiebert started yesterday, Austin A. Ramsey (4 replies) Persistent isolated probing but asymptomatic 3. Austin, One way is to just not recall the... Brent M. Hiebert 4. What I do on this cases is spoke with patient... Jose M. Illanes 5. Yeah this is essentially how I've been handling... Austin A. Ramsey 6. And thanks for the replies. Austin A. Ramsey started 5 days ago, Neda Tabatabaei (6 replies) Diagnosis 7. Thank you very much for the input Neda Tabatabaei started 6 days ago, Brent M. Hiebert (8 replies) Endo Restorative Case 8. Dr. Munce, After some prayerful... Brent M. Hiebert

top next 1. Cracked tooth. Ribbond used in the chamber. Reply via Email Direct Reply to Sender Feb 4, 2024 8:25 AM Brent M. Hiebert Following amalgam removal and access, I noted the mesial and distal cracks extended almost to the pulp chamber level. No deep probings noted clinically. Following obturation, I paper mache-ed the chamber walls with Ribbond and placed a deeper core using a dual-cure composite. Occlusion was reduced and I'm hopeful the crown will be placed soon. *I also see the distal caries. I will let the general dentist deal with that as it will get removed during the crown preparation. I completed the access fill/ribbonding at no charge to the patient. If I was doing the official buildup and would have removed caries.
@Matthew C. Davis
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate

top previous next 2. C-Shaped Canal. 2.5yr followup Reply via Email Direct Reply to Sender Feb 4, 2024 8:18 AM Brent M. Hiebert The patient returned for treatment of a different tooth so that gave me an opportunity to re-evaluate tooth 18. I cleaned and disinfected this tooth with traditional irrigation techniques and activated my irrigant with an irrisafe ultrasonic tip. Nice apical healing noted at the 2.5 year mark. It is a lone molar with no support from an adjacent tooth....hopefully, it can withstand the test of time

------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate

top previous next 3. Re: Persistent isolated probing but asymptomatic Reply via Email Direct Reply to Sender Feb 4, 2024 8:08 AM Brent M. Hiebert Austin,
One way is to just not recall the patient or reprobe the area. That way you don't know about it and you don't have to worry about it.
I should state, that I'm just joking.
If you don't suspect a crack and don't see a crack internally, I would move forward with obturating the case. I would push your recall out to a 6 to 12 month time interval. Give the body a chance to heal.
Brent
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-03-2024 03:06 PM
From: Austin A. Ramsey
Subject: Persistent isolated probing but asymptomatic
Hi All,
Wondering how people are handling these cases. For me they tend to be lower molars that often present with some type of buccal abscess, and CBCT will typically show missing buccal cortical plate. I'll clean/shape and medicate with CaOH. Patient will return 3-4 weeks later, not only feeling great, but the tissue will also look great. Then I'll find that very narrow deep probing is still present. So I re-medicate and re-eval several weeks later - the tooth still looks and feels great, but the probing persists. Of course I'm seeing no obvious cracks internally.
How are you managing these at this point?
Austin
------------------------------
Austin Ramsey D.D.S., M.S.
Chappaqua NY
------------------------------
top previous next 4. Re: Persistent isolated probing but asymptomatic Reply via Email Direct Reply to Sender Feb 4, 2024 9:27 AM Jose M. Illanes What I do on this cases is spoke with patient and explain with great detail and in a manner he could understand, that the prognosis is not good but neither bad, so recall every 6 month is needed. I'll advice you to obturate the tooth, rehab and recall
Hope you find this helpful
------------------------------
Jose Illanes
Santiago
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-03-2024 03:06 PM
From: Austin Ramsey
Subject: Persistent isolated probing but asymptomatic
Hi All,
Wondering how people are handling these cases. For me they tend to be lower molars that often present with some type of buccal abscess, and CBCT will typically show missing buccal cortical plate. I'll clean/shape and medicate with CaOH. Patient will return 3-4 weeks later, not only feeling great, but the tissue will also look great. Then I'll find that very narrow deep probing is still present. So I re-medicate and re-eval several weeks later - the tooth still looks and feels great, but the probing persists. Of course I'm seeing no obvious cracks internally.
How are you managing these at this point?
Austin
------------------------------
Austin Ramsey D.D.S., M.S.
Chappaqua NY
------------------------------

top previous next 5. Re: Persistent isolated probing but asymptomatic Reply via Email Direct Reply to Sender Feb 4, 2024 12:10 PM Austin A. Ramsey Yeah this is essentially how I've been handling them.. have a fairly extensive conversation about prognosis and let the patient decide, and then if we decide to complete treatment, schedule re-eval(s).
Do you think there's any role for perio eval/treatment in these cases?
------------------------------
Austin Ramsey D.D.S., M.S.
Chappaqua NY
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-04-2024 08:07 AM
From: Brent M. Hiebert
Subject: Persistent isolated probing but asymptomatic
Austin,
One way is to just not recall the patient or reprobe the area. That way you don't know about it and you don't have to worry about it.
I should state, that I'm just joking.
If you don't suspect a crack and don't see a crack internally, I would move forward with obturating the case. I would push your recall out to a 6 to 12 month time interval. Give the body a chance to heal.
Brent
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures

top previous next 6. Re: Persistent isolated probing but asymptomatic Reply via Email Direct Reply to Sender Feb 4, 2024 12:11 PM Austin A. Ramsey And thanks for the replies.
------------------------------
Austin Ramsey D.D.S., M.S.
Chappaqua NY
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-04-2024 09:27 AM
From: Jose M. Illanes
Subject: Persistent isolated probing but asymptomatic
What I do on this cases is spoke with patient and explain with great detail and in a manner he could understand, that the prognosis is not good but neither bad, so recall every 6 month is needed. I'll advice you to obturate the tooth, rehab and recall
Hope you find this helpful
------------------------------
Jose Illanes
Santiago

top previous next 7. Re: Diagnosis Reply via Email Direct Reply to Sender Feb 4, 2024 9:30 PM Neda Tabatabaei Thank you very much for the input
------------------------------
Neda Tabatabaei D.D.S.
Vancouver BC
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-02-2024 08:19 AM
From: Carl W. Newton
Subject: Diagnosis
Might be a good opportunity to introduce yourself to a local neurologist, if you don't already have one. My rule of referral was to give them complete information from your exam, including a differential, if possible. I always looked at it like the type of information I would really like to recieve with a referral. to me The last thing you want is to have this patient bounced around. Dr. Schwartz' recommendation of selective anesthesia is a good idea if the pain is provoked with any stimulus. Use intraosseous to further localize if it abates with either a maxillary or mandibular block. Good case for this forum.
------------------------------
Carl Newton D.D.S.,M.S.D.
Zionsville IN
(317) 258-7434
CarlNewton

top previous 8. Re: Endo Restorative Case Reply via Email Direct Reply to Sender Feb 4, 2024 8:09 AM Brent M. Hiebert Dr. Munce,
After some prayerful consideration, I have chosen to accept your apologies. I forgive you.
Brent
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
Instagram: @topgunendodontics
No financial disclosures
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 02-03-2024 12:59 PM
From: C. John Munce
Subject: Endo Restorative Case
Apologies for the duplicate postings...no idea how that happened. cjm
------------------------------
C. John Munce
Diplomate American Board of Endodontics
Sandpoint Idaho
(805)570-8666
cjohn.munce@verizon.net
-------------------------------------------------------------
*************************
-------------------------------------------------------------
Post New Message Jan 31, 2024 Discussions
started yesterday, Neda Tabatabaei (2 replies) Diagnosis 1. Neda, tying checking occlusion to make sure not... Nicole M. Yingling 2. Neda, your testing was conclusive. The... Richard S. Schwartz started 4 days ago, Brent M. Hiebert (5 replies) Surgical ICR Repair 3. Beautiful cases and great documentation, Brent.... Nicole M. Yingling started 13 days ago, Cami E. Ferris-Wong (2 replies) Frustrating morning... 4. Follow-up on that moving target case... What a... Cami E. Ferris-Wong

top next 1. Re: Diagnosis Reply via Email Direct Reply to Sender Jan 31, 2024 7:57 AM Nicole M. Yingling Neda, tying checking occlusion to make sure not heavy or any interferences then palpate muscles of mastication for tender spots, bilaterallyt. I discover a lot of myofascial pain patients that present with endo symptoms. Good luck!
------------------------------
Nicole Yingling D.M.D.
Chambersburg PA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 01-30-2024 10:50 PM
From: Neda Tabatabaei
Subject: Diagnosis
41 year old female patient is experiencing pain on lower right from 2-3 weeks ago, pain radiates to her right ear as well. She is taking antibiotic prescribed by her general dentist . Also, she said she is taking pain killer but it does not do anything for her.
She responded normal to all endodontic tests including cold, probing was normal. The only symptom was feeling slight pain 1-2minutes after bite test on lower first premolar.
I included a few CBCT snapshots which shows lateral lucency associated with both lower premolars. Also, lower first premolar has two canals.
Is that perio? Is there any other tests I need to do?
Thank you for your help in advance.
------------------------------
Neda Tabatabaei D.D.S.
Vancouver BC
------------------------------

top previous next 2. Re: Diagnosis Reply via Email Direct Reply to Sender Jan 31, 2024 12:50 PM Richard S. Schwartz Neda, your testing was conclusive. The radiography is not very conclusive. As Nicole said, I'd be looking for a non-endodontic source of the pain. If you can consistently reproduce delayed pain from the bite test, and the patient is convinced it is from that tooth, you could retest after anesthesia. But it doesn't appear to be an endodontic problem. I'd probably refer to a head and neck pain specialist.
Rick
------------------------------
Richard Schwartz D.D.S.
San Antonio TX
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 01-30-2024 10:50 PM
From: Neda Tabatabaei
Subject: Diagnosis
41 year old female patient is experiencing pain on lower right from 2-3 weeks ago, pain radiates to her right ear as well. She is taking antibiotic prescribed by her general dentist . Also, she said she is taking pain killer but it does not do anything for her.
She responded normal to all endodontic tests including cold, probing was normal. The only symptom was feeling slight pain 1-2minutes after bite test on lower first premolar.
I included a few CBCT snapshots which shows lateral lucency associated with both lower premolars. Also, lower first premolar has two canals.
Is that perio? Is there any other tests I need to do?
Thank you for your help in advance.
------------------------------
Neda Tabatabaei D.D.S.
Vancouver BC
------------------------------

top previous next 3. Re: Surgical ICR Repair Reply via Email Direct Reply to Sender Jan 31, 2024 7:59 AM Nicole M. Yingling Beautiful cases and great documentation, Brent. Thanks for sharing!
------------------------------
Nicole Yingling D.M.D.
Chambersburg PA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
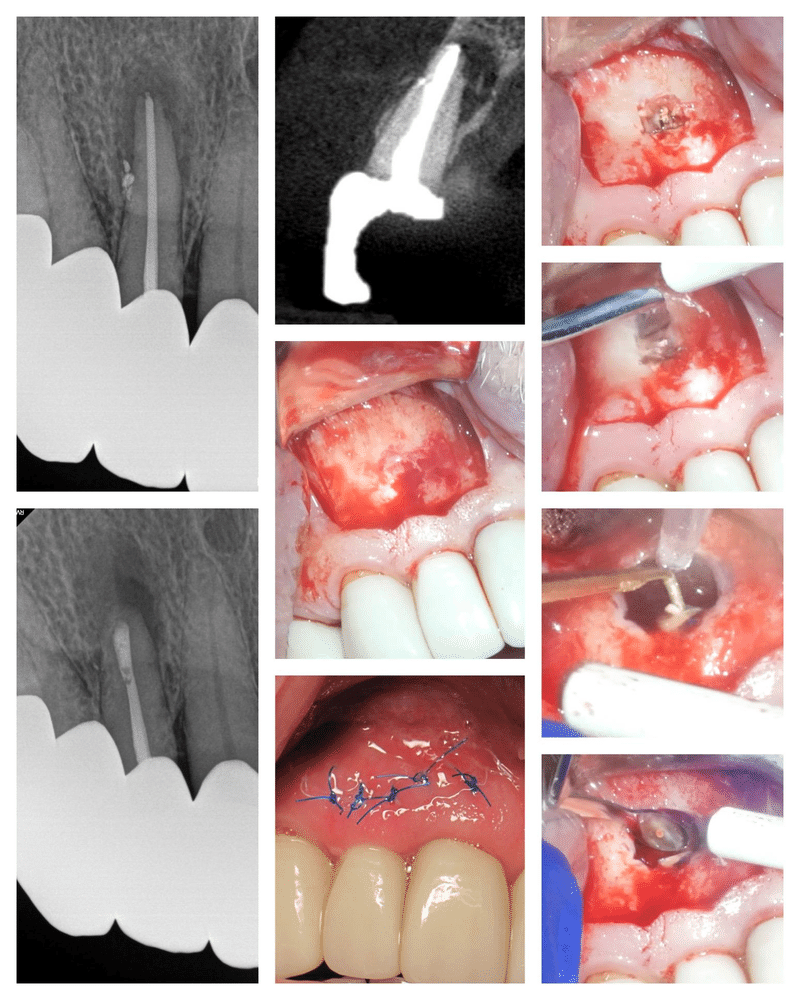
Sent: 01-27-2024 06:13 PM
From: Brent M. Hiebert
Subject: Surgical ICR Repair
45 y/o male
Tooth 19. Prev Tx/NAT. ICR defect on the buccal.
Surgical repair. There was quite a bit of bone ingrowth into the defect that had to be removed. I restored this one with Fuji II RMGI.





------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------

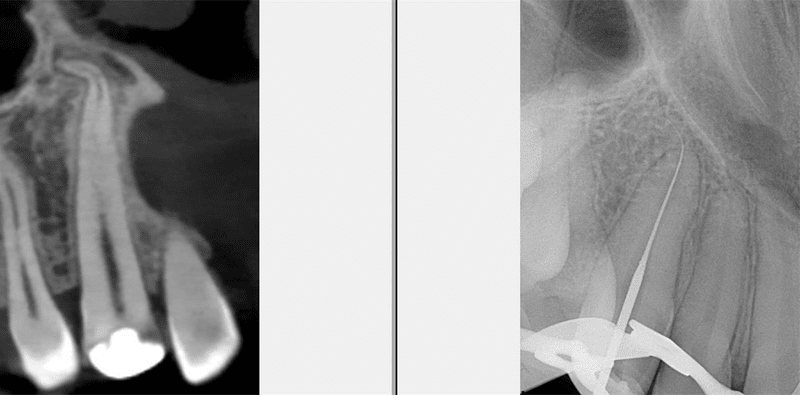
top previous 4. Re: Frustrating morning... Reply via Email Direct Reply to Sender Jan 31, 2024 2:46 PM Cami E. Ferris-Wong Follow-up on that moving target case... What a difference 1mg of Xanax makes!! She came back nice and drowsy, no shaking, easy anesthesia, but it was still a bear to try to get in that ML canal. Here is a reminder of the inter-op CBCT I took with CH in the MB canal:

I used ultrasonic to open the main orifice toward the lingual, still shocked that there was no opening visible. I saw a little spot and kept following it, though I couldn't get a file in. I went ahead and packed the ML and D hoping I'd squirt a little of the white sealer deeper and could follow that trail:

I nearly gave up several times but kept following the trail until finally, I could get a file in (see the small opening opposite the already filled ML). So glad I did... here is the result (bummed about the sealer puff, I did pump the cone a little in a victory dance sort of way).

Now the question of the day is... If I hadn't taken a pre-op CBCT and the subsequent intra-op CBCT, would I have tried so hard? My honest answer, probably not. I could have convinced myself that there was really maybe only one mesial canal or that they likely merge. But the CBCT tells the real story and keeps me honest, making me a better endodontist.
Smiles,
Cami
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 01-18-2024 01:14 PM
From: Jonathan A. Mason
Subject: Frustrating morning...
🙏 Brutal cases. Awesome effort on both of them! Moving targets are so hard. Hopefully they heal just fine in spite of the challenges. Which of you is taking the Xanax next time? 😂
------------------------------
Jon Mason
You are subscribed to "AAE Discussion Open Forum" as toho_dental_club@yahoo.co.jp. Getting to many emails? Adjust your Community Notifications to the Weekly Digest option. To unsubscribe from this community discussion, go to Unsubscribe.
**********************************************************************************
Post New Message Jan 29, 2024 Discussions
started 22 hours ago, Brent M. Hiebert (0 replies) Endo Restorative Case 1. Tooth 21: Endo restorative case. Laser used for... Brent M. Hiebert started 2 days ago, Brent M. Hiebert (1 reply) Surgical ICR Repair 2. A 5 day follow up shows nice tissue healing. ... Brent M. Hiebert started 24 days ago, Cami E. Ferris-Wong (6 replies) CBCT surprise 3. Cami--What if the crown had not previously... C. John Munce 4. Thanks John, That is a great solution! You... Cami E. Ferris-Wong

top next 1. Endo Restorative Case Reply via Email Direct Reply to Sender Jan 29, 2024 8:36 AM Brent M. Hiebert
Tooth 21: Endo restorative case. Laser used for cleaning/disinfection and gingivectomy. Buccal restored with luxacore z. PostCore buildup to finish things off. Apical bifurcation for an extra challenge. #topgunendodontics
video of case available on Instagram

------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate

top previous next 2. Re: Surgical ICR Repair Reply via Email Direct Reply to Sender Jan 29, 2024 1:12 PM Brent M. Hiebert A 5 day follow up shows nice tissue healing.


------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 01-27-2024 06:13 PM
From: Brent M. Hiebert
Subject: Surgical ICR Repair
45 y/o male
Tooth 19. Prev Tx/NAT. ICR defect on the buccal.
Surgical repair. There was quite a bit of bone ingrowth into the defect that had to be removed. I restored this one with Fuji II RMGI.





------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------

top previous next 3. Re: CBCT surprise Reply via Email Direct Reply to Sender Jan 29, 2024 12:47 AM | view attached C. John Munce Cami--What if the crown had not previously snapped off, and the overall length turned out to be say 38mm+? I encountered that a number of times, and attached is my step-by-step work-around. cjm
------------------------------
C. John Munce
Diplomate American Board of Endodontics
Sandpoint Idaho
(805)570-8666
cjohn.munce@verizon.net
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 01-27-2024 11:31 AM
From: Justin Wu
Subject: CBCT surprise
Wow! Im surprised you were able to get a 20 to the terminus! I don't take many post op cbcts but a case like this would have been tempting(not sure if it is really warranted).
Original Message:
Sent: 1/26/2024 6:05:00 PM
From: Cami E. Ferris-Wong
Subject: RE: CBCT surprise
Here is the follow-up to this CBCT surprise. I was lucky that his tooth has previously broken off because if it hadn't I would have been in trouble. The length turned out to be a cool 31mm. I was able to get pre-curved 10 and 15 file to length and then heat treated tapers (20/ .04) to 1-2mm back. Then my (pre-curved) 20 K-file went to length. Ran GentleWave (no disclosures), fused two cones together to get more length and used my long pluggers to pack. Not gonna lie, I was stressed going in, and the patient was an angsty teen so that didn't help. But all is well!

Smiles,
Cami
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
top previous 4. Re: CBCT surprise Reply via Email Direct Reply to Sender Jan 29, 2024 12:42 PM Cami E. Ferris-Wong Thanks John,
That is a great solution! You should make a book with all of your "work arounds." You are truly the MacGyver of Endo!!
Smiles,
Cami
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------

Original Message:
Sent: 01-29-2024 12:46 AM
From: C. John Munce
Subject: CBCT surprise
Cami--What if the crown had not previously snapped off, and the overall length turned out to be say 38mm+? I encountered that a number of times, and attached is my step-by-step work-around. cjm
------------------------------
C. John Munce
Diplomate American Board of Endodontics
Sandpoint Idaho
(805)570-8666
cjohn.munce@verizon.net
You are subscribed to "AAE Discussion Open Forum" as toho_dental_club@yahoo.co.jp. Getting to many emails? Adjust your Community Notifications to the Weekly Digest option. To unsubscribe from this community discussion, go to Unsubscribe.
**********************************************************************************
Post New Message Jan 13, 2024 Discussions
started 19 hours ago, Brent M. Hiebert (1 reply) 4 apical surgery cases 1. No disclosures. I posted videos of all cases on... Brent M. Hiebert 2. Outstanding surgical treatments Brent! I'd love... Brett E. Gilbert started 10 days ago, Pablo Salmeron (7 replies) Numbness / Paresthesia 3. Hi Cami, Thank you for taking the time to... Pablo Salmeron

top next 1. 4 apical surgery cases Reply via Email Direct Reply to Sender Jan 13, 2024 11:26 AM Brent M. Hiebert No disclosures.
I posted videos of all cases on Instagram for those interested.
7 Apical Surgery with bone graft. Submarginal incision. Acteon piezotome cube utilized. Retrofitted with BC putty.

10 Apical Surgery. Submarginal incision. Acteon piezotome cube implemented for osteotomy and root resection. Refined resection with Lindemann bur. Retro prep with KiS US tip. Retrofit with bc putty. Bone graft placed. Closed with 6-0 polypropylene sutures. 96hr followup shows good tissue healing. I'll have her back in 6 months for followup.

7 apical surgery. Submarginal incision implemented. Root resection with Acteon piezotome cube. Retro prep with US KiS tips. Retro fill with bc putty. Sutures: 5-0 polypropylene and 6-0 PTFE. 1 week followup shows nice tissue healing.

14 apical surgery. This was a second apico on the tooth. A more aggressive/radical resection and deeper retro prep were done on the MB root due to persistent apical periodontitis. During the procedure I noted a crack on the lingual - which I was able to remove with further resection. Retro-filled with BC sealer, BC putty and bone graft.

@Charles T. Maupin @Austyn C. Grissom @Adham A. Azim @Joseph C. Stern @Gordon S. Lai @B. Craig Anderson @Alan H. Gluskin @Cyrous Ardalan @Stephen P. Niemczyk @Jason W. Kwok @Mohamed I. Fayad @Richard A. Rubinstein @Frederic Barnett @Cami E. Ferris-Wong @Jason F. Foreman @Justin Y. Wu @Kevin B. Stewart @Katie R. Kickertz @Harley B. Grandin @Richard S. Schwartz @Benjamin Schwabe @Elizabeth Shin Perry @Sameer D. Jain @Kip M. Sterling @Ahmed B. Salman @Pablo Salmeron @Brett E. Gilbert
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate

top previous next 2. Re: 4 apical surgery cases Reply via Email Direct Reply to Sender Jan 13, 2024 4:12 PM Brett E. Gilbert Outstanding surgical treatments Brent! I'd love to incorporate the cube into my practice. I'll reach out to learn more about your experience with it!
------------------------------
Brett E. Gilbert, D.D.S.
Diplomate, American Board of Endodontics
King Endodontics, LLC
Niles, IL
847-588-7890
www.kingendo.com
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 01-13-2024 11:26 AM
From: Brent M. Hiebert
Subject: 4 apical surgery cases
No disclosures.
I posted videos of all cases on Instagram for those interested.
7 Apical Surgery with bone graft. Submarginal incision. Acteon piezotome cube utilized. Retrofitted with BC putty.

10 Apical Surgery. Submarginal incision. Acteon piezotome cube implemented for osteotomy and root resection. Refined resection with Lindemann bur. Retro prep with KiS US tip. Retrofit with bc putty. Bone graft placed. Closed with 6-0 polypropylene sutures. 96hr followup shows good tissue healing. I'll have her back in 6 months for followup.

7 apical surgery. Submarginal incision implemented. Root resection with Acteon piezotome cube. Retro prep with US KiS tips. Retro fill with bc putty. Sutures: 5-0 polypropylene and 6-0 PTFE. 1 week followup shows nice tissue healing.
14 apical surgery. This was a second apico on the tooth. A more aggressive/radical resection and deeper retro prep were done on the MB root due to persistent apical periodontitis. During the procedure I noted a crack on the lingual - which I was able to remove with further resection. Retro-filled with BC sealer, BC putty and bone graft.

@Charles T. Maupin @Austyn C. Grissom @Adham A. Azim @Joseph C. Stern @Gordon S. Lai @B. Craig Anderson @Alan H. Gluskin @Cyrous Ardalan @Stephen P. Niemczyk @Jason W. Kwok @Mohamed I. Fayad @Richard A. Rubinstein @Frederic Barnett @Cami E. Ferris-Wong @Jason F. Foreman @Justin Y. Wu @Kevin B. Stewart @Katie R. Kickertz @Harley B. Grandin @Richard S. Schwartz @Benjamin Schwabe @Elizabeth Shin Perry @Sameer D. Jain @Kip M. Sterling @Ahmed B. Salman @Pablo Salmeron @Brett E. Gilbert
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
top previous 3. Re: Numbness / Paresthesia Reply via Email Direct Reply to Sender Jan 13, 2024 12:07 AM Pablo Salmeron Hi Cami,
Thank you for taking the time to answer. As medicine is not an exact science and patients' anatomies differ from one another, we must keep in mind that permanent or temporary paresthesia due to nerve injury is one of the complications that can occur when we do an IAN block. It is statistically likely that a long professional career will bring about such mishaps sooner or later to us.
Thank you again for sharing your experience; I really appreciate it.
Kind regards,
------------------------------
Dr. Pablo Salmeron, D.M.D., M.Sc., Ph.D.
Consultant Endodontist.
Dubai, UAE.
-----------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 01-12-2024 05:37 PM
From: Cami E. Ferris-Wong
Subject: Numbness / Paresthesia
Hi Pablo,
This is great news! I was going to chime in earlier with an anecdote... About 10 years ago, only a few months after I started using articaine for IANB, I had a patient who had long-term (several months) paresthesia. The interesting thing was that she came in saying that her dentist could never get her numb for procedures and she hated having dental work done because she could always feel it when he was drilling. I gave my anesthetic and she was profoundly numb during the procedure for the first time in her life. She called back saying that I did such a good job she was still numb a week later. I was horrified and considered never using articaine again. But within a couple weeks it was barely noticeable to her, and we kept her on recall with mapping of the area so that she could see it was getting better each time. Eventually it went away completely. I think she was such a good sport about it because she was grateful that the RCT went so well. Because of that, I kept using articaine for blocks and (knock on wood) haven't had an issue since.
So, the moral of the story is that it is more likely just a timing issue rather than attributed to the use of the articaine. Most of us that practice more than 10 years probably have at least one story to share.
The one other anecdote I will mention is that you do not want to use the articaine for a lingual infiltration in the lower molar region. When I first started using articaine for the block, I would also give the lingual supplemental injection (just enough to blanch the tissue) with it and I had issues with it creating an ulceration that is pretty painful for a couple of weeks. Switch to Lido 2% 1:100 for that injection and you will have no problems.
Smiles,
Cami
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
****************************

The extraoral sinus was treated differently inside the same tooth







------------------------------
Abu Saeed Harun B.D.S., M.S.
Chattagram
------------------------------
**********************************************************************************
--------------------------------------------------------------------------------------
top next 1. Related to Austin Ramsey's question

Richard S. Schwartz Here are a few SEM images from the project several of us are doing with Gary Carr. When a patient has a tooth that needs to be extracted, if they consent we instrument by some method, irrigate with one of various methods, extract, drop it in formalin and send it to Gary for SEM imaging. I'm getting closer to putting together a lecture to present the findings, but here is a small sample. We are finding all the "advanced" irrigation devices provide a "cleaner" looking canal than passive needle irrigation. There are certain qualifiers which I'll discuss in my lecture.
The first image is from the midroot of a canal instrumented to size 30 with minimal irrigation with 6% bleach and nothing else. The predentin is largely intact and covered in many areas with smear layer. There are no overt signs of microorganisms, but there are almost certainly some embedded in the residual smear layer. You can also see pulpal remnants and some debris, with little evidence of dentinal tubules.
The second image is from the midroot of a tooth also instrumented to size 30 with bleach and EDTA with laser irrigation, in this case Fotona. There is some predentin and debris present, but many exposed dentinal tubules. When you look at the surface at higher magnification most of the inter- and intra-tubular dentin was removed. The whole surface was largely demineralized. There was little evidence of microbes. I chose the midroot for these examples because the difference is fairly dramatic. Not surprisingly, it is less dramatic in the apical 1/3.
The final image is from a tooth in which there was a deep split and a laser was used. There was no instrumentation in the canal that is shown. You can see it is filled with pulp tissue, RBCs and debris. The laser had minimal effect. This was also generally true with all the irrigating devices. They were really only effective in canals where an instrument had at least partially cleaned the canal.
We have found the advanced irrigation devices all seem to clean the canals better than needle irrigation. Does it make a difference as far as success and failure? We don't know. As for me, the deeper we get into this project, it makes me feel better using one of the devices, so I use them as much as possible. I don't know if it makes a difference, but it makes me feel better. We have also found that the invivo results are much different that if you use extracted teeth, which is what you see in the published SEM studies.
Rick



------------------------------
Richard Schwartz D.D.S.
San Antonio TX
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate
top previous next 2. Re: Decoronation recall
Dec 17, 2023 2:06 PM

Marc I. Semper Dear Rick, of course you're always wiser in hindsight. But I notice a few points that could have stood in the way of a replacement reorption. Based on the periapical radiographs, I suspect that the tooth root was not completely reduced below the level of the surrounding alveolar bone (2 mm recommended). Furthermore, it can be discussed whether it is better not to apply a dressing (CaOH2 in your case?), but rather to allow it to fill with blood. This might be important, as the blood clot is organized from the surrounding tissues. A closed procedure, i.e. the preparation of a flap, is of course mandatory here. Irrigation is another topic. Some might remember Malmgren, who recommende saline, not sodium hypochlorite. Just my humble opinion. Best, Marc
------------------------------
Marc I. Semper
ESE Certified Member, AAE International Specialist Member
Bremen Germany
+4915120961772
marcsemper@icloud.com
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 12-14-2023 08:53 PM
From: Richard Schwartz
Subject: Decoronation recall
The patient had trauma, #9 ankylosed. He wasn't a good candidate for an autotransplant so we went to our second choice, decoronation. I removed the gutta percha and performed it 21 months ago just before the start of orthodontics. I sectioned off the crown and added some composite to the apical portion of the crown and the orthodontist bonded it on the orthodontic wire. Ideally we would like to see bone grow over the root. That didn't happen here, but it does have nice soft tissue for a pontic site. He is 14 now. The braces are coming off in a few weeks and his restorative dentist will make him a single wing Maryland Bridge that will hopefully carry him through until he is old enough for an implant.
Rick

------------------------------
Richard Schwartz D.D.S.
San Antonio TX
------------------------------
top previous next 3. Re: Decoronation recall
Dec 17, 2023 2:39 PM
Richard S. Schwartz Hi Mark, I believe I did reduce it 2 mm below the crest, or at least, it looked that way clinically. It doesn't look that way in the 3rd radiograph, but it does in the 4th. There was gutta percha in the canal. I was able to remove most of it although there was a little residual of something. I didn't place CaOH. I left the canal open and it filled with blood. I did irrigate with saline. Basically I tried to follow Malmgren's recommendations. Thanks for your comments. It seems to be hard to get anyone to comment on anything other than ept and cracked teeth.
Rick
------------------------------
Richard Schwartz D.D.S.
San Antonio TX
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 12-17-2023 02:05 PM
From: Marc I. Semper
Subject: Decoronation recall
Dear Rick, of course you're always wiser in hindsight. But I notice a few points that could have stood in the way of a replacement reorption. Based on the periapical radiographs, I suspect that the tooth root was not completely reduced below the level of the surrounding alveolar bone (2 mm recommended). Furthermore, it can be discussed whether it is better not to apply a dressing (CaOH2 in your case?), but rather to allow it to fill with blood. This might be important, as the blood clot is organized from the surrounding tissues. A closed procedure, i.e. the preparation of a flap, is of course mandatory here. Irrigation is another topic. Some might remember Malmgren, who recommende saline, not sodium hypochlorite. Just my humble opinion. Best, Marc
------------------------------
Marc I. Semper
ESE Certified Member, AAE International Specialist Member
Bremen Germany
+4915120961772
marcsemper@icloud.com
top previous next 4. Re: Today's EPT failure, here we go again
Dec 17, 2023 8:53 AM

Justin Y. Wu Nate,
You pose some interesting points.
Going back to Rick's case, let's say access #25 and it happens to be vital, you do your VPT and send for biopsy. Your OMFS more than likely will curette the bone clean based on the assumption that this lesion is non-odontogenic in origin(OMFS are big on this in my experience). So what would you do in 6 months if a radiolucency returns and your EPT is still reading vital?
To me the benefit of VPT in this case is minimal which is why I think the RCT would be the way to go regardless. An RCT is not much more damaging to the tooth, possibly beneficial if you can place a deep resin/fiber post and you help rule out diagnosis questions in the future.
------------------------------
Justin Wu D.D.S.
Santa Rosa CA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 12-15-2023 09:40 AM
From: Nathan A. Dinsbach
Subject: Today's EPT failure, here we go again
Hi Rick, I think this is a great discussion to have for the benefit of some of the newer endodontists / residents. Sorry if this is a long post… you asked what I would do if the patient you presented at the top of this thread presented to me.
I, like many of us endodontists, like to think and talk with patients in terms of probability. Much like the AAE prognosis categories are favorable, questionable and unfavorable – in a complicated scenario I will inform a patient that I believe that s/he has either a low probability of success/healing, a coin-toss probability of success/healing, or a high probability of success/healing. We then discuss the reasons why I chose that level of probability. I also like to think in terms of probability regarding the etiology of the pathosis present.
In the scenario you presented above, we see a large radiolucent area focused at the apex of #25 , that is large enough to involve adjacent teeth. Playing the probability game, the large majority of radiolucencies are of odontogenic origin, and most of these are due to pulpal pathosis. Obviously, we perform our tests to make sure we have a sound diagnosis and that we are not in the "non-odontogenic" realm of pathosis. In the case above, after doing the tests you mentioned, I would say something like, "Usually the issue we see on your radiograph is related to pulp tissue in a tooth that has died. None of our tests are perfect which is why we perform multiple tests. I would not have expected this tooth to have responded to the electric test. However, the most likely reason for the pathosis we see (pointing to the radiograph) is due to bacteria in the pulp space. I would recommend a root canal procedure. However, if I open into the tooth and see healthy tissue, I will stop and place a special medicated filling that will allow the pulp tissue to remain healthy." I wouldn't say it at this point, but if I did find vital tissue, at the end of the appointment I would recommend a biopsy.
Now, with high probability I'm going to guess what you're thinking. "If you're in the tooth and you're going to recommend biopsy, why wouldn't you complete the endodontic therapy and maybe fill the canal with MTA?" That's a fair question. I'm going to answer your question by posing two questions. I may be kicking a hornet's nest… and maybe need to continue this conversation in a different thread.
Do we know of a specialty in dentistry that devitalizes multiple teeth in one setting? And if so, do these specialists have studies on how many of these teeth subsequently become necrotic? The answer is yes and yes. We know that LeFort procedures devitalize teeth… and in the OMFS literature, only 1% to 5% of these teeth become necrotic.
Back to your case above – if I opened and found perfectly vital tissue, I would close with bioceramic material and resin and refer for a biopsy. If that tooth were to become necrotic in the future… I can perform the endodontic therapy at that point. But based on the literature we have for a tooth with a healthy vital pulp, the probability of pulp necrosis after devitalization is low.
In the case I presented, I agree that the EPT test does not tell us if a pulp is vital. We also know that the cold test does not reliably tell us if the pulp is vital (for example, during diagnostic testing of a tooth, I place cold on a tooth and it triggers a very elevated, throbbing response... yet when I access the tooth, the tissues are necrotic. I know I'm not the only one that has seen this...). In the case of #15 that I presented, the EPT showed that the pulp was responsive. Given that there were no other signs and symptoms in the case I presented, if tooth #15 would have not responded at all to the EPT, and given the fractured marginal ridge and recurrent caries, I would have then recommended endodontic therapy.
That's my long-winded $0.02
------------------------------
Nathan Dinsbach D.D.S.,M.S.D.
Mooresville NC
top previous next 5. Re: Today's EPT failure, here we go again Reply via Email Direct Reply to Sender Dec 17, 2023 9:26 AM Kyle Williams I appreciate this discussion you all are having. I am a second year endodontic resident. My research project for my thesis manuscript is focused on this very topic. We are comparing the physics between two EPT units, recording the frequency of false positives, and investigating the possibilities for why they happen. The observations are being made by direct visualization under the microscope of the pulp chamber/canals after accessing, as well as histologically in extracted teeth that were tested with EPT prior to the removal. A couple of my personal observations since starting the study that are not supported at this point, but in my opinion are interesting;
A tooth with a necrotic pulp chamber, but vital tissue in the canal space/s, will respond to EPT.
In a multicanal tooth if 2 of the 3 canals are necrotic/empty, but one canal is vital/bleeding, it responds to EPT.
For no response to EPT the necrotic tooth usually is empty/dry.
Still a ways to go, but hoping to get published at some point, fingers crossed, so be on the lookout. Happy Holidays!
S. Kyle Williams
------------------------------
Kyle Williams D.D.S.
Charleston SC
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 12-15-2023 08:02 PM
From: Jeffrey H. Janian
Subject: Today's EPT failure, here we go again
Rick,
I anticipate I didn't really have to use a super fast increase to 80, and could've used a slow increase to 80. (Not to mention I've only done this 5–6x because the situation comes up rarely.)
My rationale at going at a fast rate was to not even give them a chance to let go because, in their brain, they think it's going to take longer to feel it. They might drop it just because they were worried about what I was asking them to do: feel pain.
I'm definitely curious if this has any valid use, or I just happened to get the results I did.
If it doesn't work out when you try, I'll buy you (and the patient) a meal : )
-Jeff
Jeffrey H Janian, DDS
Sent from my iPad
Original Message
Sent: 12/14/2023 8:41:00 PM
From: Richard S. Schwartz
Subject: RE: Today's EPT failure, here we go again
Hi Jeff, It will make me a little nervous, but I'll try your technique next time I get a chance.
Rick
------------------------------
Richard Schwartz D.D.S.
San Antonio TX
top previous next 6. Re: Retreatment Case Reply via Email Direct Reply to Sender Dec 17, 2023 2:52 PM

Noah Chivian A belated thank you for supporting my position. Also a belated Happy Chanukah
Noah
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 11/17/2023 9:16:00 AM
From: Brent M. Hiebert
Subject: Retreatment Case
This was a case from a few days ago. I've had a lot of tough retreatment cases lately (woe is me ;-) ). Thankfully, for this case, once I jack-hammered out the amalgam, this case was fairly straight forward.
During my residency at Loma Linda (circa 2016ish), Dr. Torabinejad @Mahmoud Torabinejad would always tell us to ask the question, "can we improve on what's been done?" when evaluating retreatment cases. You can see from the imaging for this case they forgot to obturate most of the canal space (inadequate initial RCT). We know that the obturation is generally a reflection on the type of cleaning of the canal system. So it was not difficult to improve this case.


------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
-----------------------------
top previous 7. Re: Biolase warranty and cost analysis Reply via Email Direct Reply to Sender Dec 17, 2023 11:30 AM

Austin A. Ramsey Hey Brandon - I realize this thread is a bit old, but wondering if there are any updates here? My office is thinking about incorporating laser into the flow so trying to learn a little more from others' experiences. I was also wondering how those who take insurance go about charging/billing for the added service.
Thanks here and for posting in general Brandon, I appreciate the time you give on the forum!
Austin
------------------------------
Austin Ramsey D.D.S., M.S.
Chappaqua NY
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 08-26-2022 07:56 PM
From: Brandon G. Seto
Subject: Biolase warranty and cost analysis
I don't know...that's a tough question to answer. Like I said, I have been happily using the laser for the last 10 months. To me, I see a big improvement in the visual cleanliness over passive ultrasonics. (Comparing it to Gentlewave would be a whole separate discussion!)
It integrates nicely with my clinical flow and I've found it very easy to incorporate.
My fear is the cost of the warranty reflects the fragility of the machine. I've read of expensive Gentlewave repairs and their warranty is the similar, BUT the discount they offer with a higher volume of procedures would give me confidence in using it. Right now I'm looking at my laser, thinking of whether to use it on a case and wondering if this is going to be the case that starts the trunk fiber to crack. So now I've lost confidence in the machine and I'm second guessing whether to use it. Personally, I don't like have a machine that I have to treat with kid-gloves.
What has been your experience with the laser?
Brandon
------------------------------
Brandon Seto, D.D.S., M.S.D.
Diplomate, American Board of Endodontics
Santa Monica, CA
You are subscribed to "AAE Discussion Open Forum" as toho_dental_club@yahoo.co.jp. Getting to many emails? Adjust your Community Notifications to the Weekly Digest option. To unsubscribe from this community discussion, go to Unsubscribe.
***********************************************************************

Brent M. Hiebert This tooth had significant mesial caries along with class V buccal caries that wrapped around to the distal . Once caries were removed and canals accessed, I held the canal space with GP cones and free flowed Fuji II GI with a 24 gauge accudose needle tube. After that, I was able to focus on the RCT.
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate
top previous next 2. Re: REGEN head-scratcher case

This is an interesting case, thanks for posting it! I'm not sure why the distal root is regressing, but I personally would not try again for regen on it. My next step would be to access again, go through disinfection protocol with activated irrigants, pack the mesial roots routinely. I'd then place collacote in the distal root to give myself a backstop at the root end to pack against, use bioceramic putty for the apical 5mm or so, place a GI liner and then a nice deep core. This kid has been through enough. One-step apexification is predictable and I would think the tooth will be successful for decades if not a lifetime given the way it presents now.
Keep us posted on what you do!
Smiles,
Cami
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate ---
Original Message:
Sent: 12-09-2023 12:52 PM
From: Omar Gabr
Subject: REGEN head-scratcher case
13 yr old male came in with CC of pain on eating and swelling. Clinical evaluation showed #31 intraoral swelling along with drainage through sulcus. Radiographic eval showed #31 attempted pulpotomy and restoration with large PARL and incomplete root development w/ wide open apices. Decided to go for GER to hopefully gain root length and dentin thickness following AAE's recommended protocol using CaOH.
There were a couple of findings that got me scratching my head, for some reason the CaOH in the M roots never resorbed and the root continued development around it. The PARL was almost completely resolved in the 6MRC, but I recently did a 12MRC and the lesion definitely increased in size!
What would you do moving forward? My plan is to do NSRCT on the M root and give the D root another try with GER to increase survivability.
Please find comments below each pic/radiograph





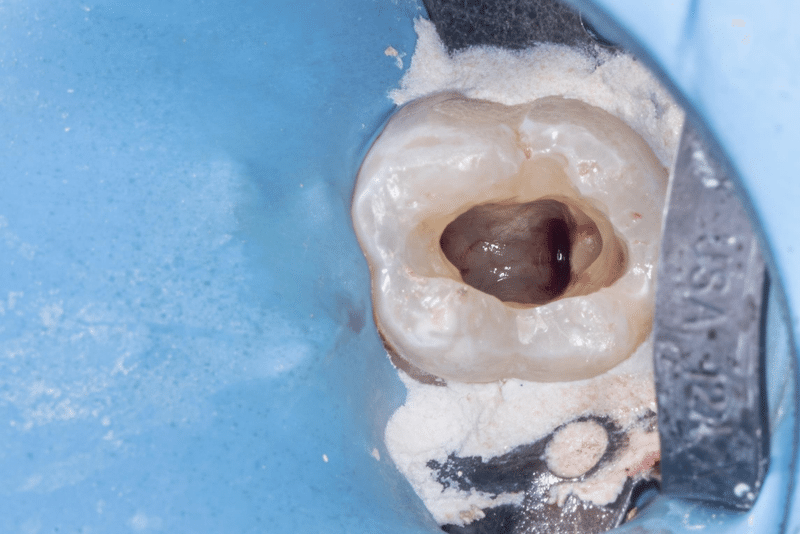




------------------------------
Omar Gabr, DDS
Resident (2024)
University of Minnesota
www.instagram.com/endobygabr
------------------------------
top previous next 3. Re: REGEN head-scratcher case
Dec 10, 2023 10:24 AM Cami E. Ferris-Wong I forgot to mention in my earlier post, I think that CH in the mesial root is most certainly just stuck in the isthmus between the canals. That is why it didn't flush out or resorb away.
Smiles,
Cami
------------------------------
Cami Ferris-Wong, DDS
Diplomate, Board of Endodontics
Boston University Endo 2000
Santa Barbara, CA
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate ----
Original Message:
Sent: 12-09-2023 12:52 PM
From: Omar Gabr
Subject: REGEN head-scratcher case
13 yr old male came in with CC of pain on eating and swelling. Clinical evaluation showed #31 intraoral swelling along with drainage through sulcus. Radiographic eval showed #31 attempted pulpotomy and restoration with large PARL and incomplete root development w/ wide open apices. Decided to go for GER to hopefully gain root length and dentin thickness following AAE's recommended protocol using CaOH.
What would you do moving forward? My plan is to do NSRCT on the M root and give the D root another try with GER to increase survivability.
Please find comments below each pic/radiograph


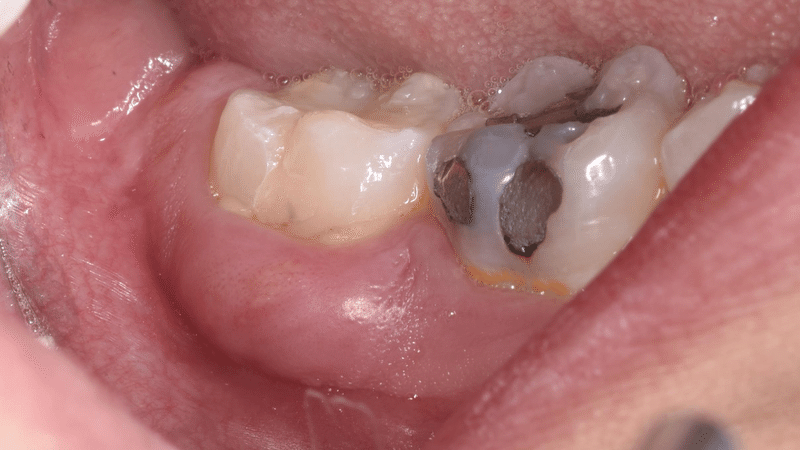
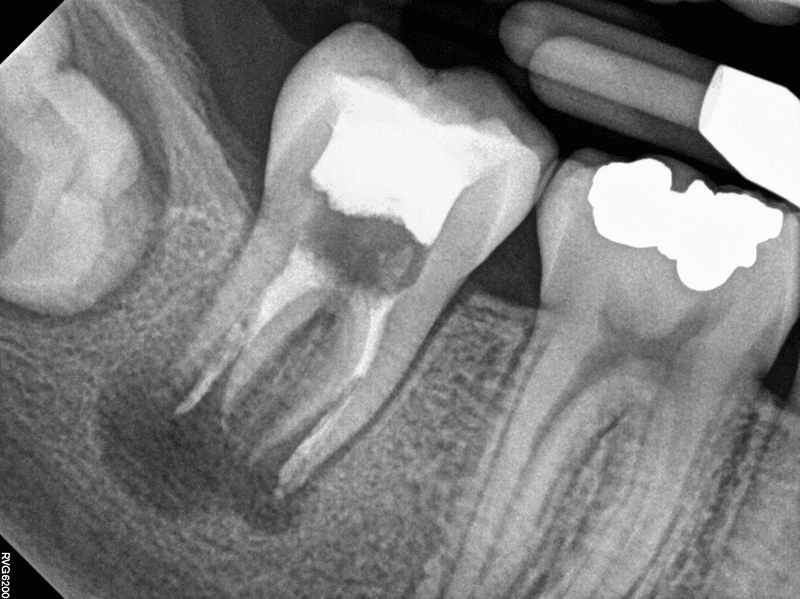

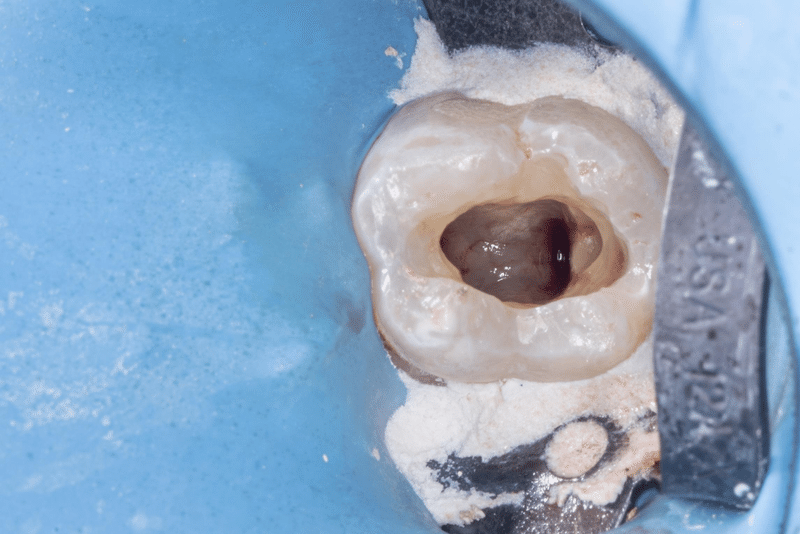




****************************************************************************
Forum
Post New Message Nov 28, 2023 Discussions
started 23 hours ago, Brent M. Hiebert (0 replies) Deep recurrent caries on 2-unit bridge... (dun dun dun sound effect) 1. Below is a case I treated last week. 77 y/o... Brent M. Hiebert started 7 days ago, Katherine Fry Hidi (2 replies) #30 pulpal necrosis with history of AAA on a 7 yr old girl 2. I don't know how her behavior will be. ... Katherine Fry Hidi
top next 1. Deep recurrent caries on 2-unit bridge... (dun dun dun sound effect)
Reply via Email Direct Reply to Sender

77 y/o male with deep recurrent mesial caries on tooth 12. Teeth 12 and 13 are a 2-unit bridge. The patient wanted to retain the bridge if possible and the referring dentist gave no information or guidance for the case. So this is what we did:

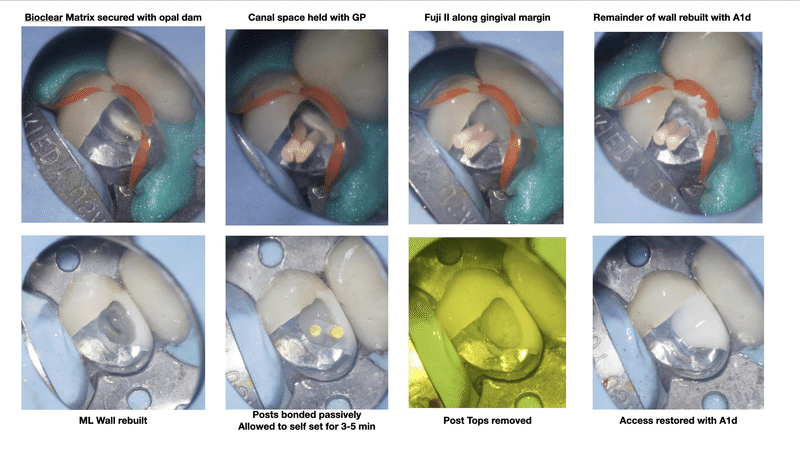


------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate
**********************************
Forum
Post New Message Nov 29, 2023 Discussions started yesterday, Brent M. Hiebert (2 replies) Deep recurrent caries on 2-unit bridge... (dun dun dun sound effect) 1. That's one hellova service!! Robert J. Cavalieri 2. Nicely-done under very challenging conditions... C. John Munce started 9 days ago, A.K. Bobby Mallik (3 replies) Stella Life Promotional video 3. Bobby, Just checking in to see how you are... Brent M. Hiebert 4. I've yet to regain a sense of calmness since you... Douglas N. Robertson top next 1. Re: Deep recurrent caries on 2-unit bridge... (dun dun dun sound effect)

Reply via Community View Thread Recommend Flag as Inappropriate ----
Original Message:
Sent: 11/28/2023 8:43:00 AM
From: Brent M. Hiebert
Subject: Deep recurrent caries on 2-unit bridge... (dun dun dun sound effect)
Below is a case I treated last week.
77 y/o male with deep recurrent mesial caries on tooth 12. Teeth 12 and 13 are a 2-unit bridge. The patient wanted to retain the bridge if possible and the referring dentist gave no information or guidance for the case. So this is what we did:

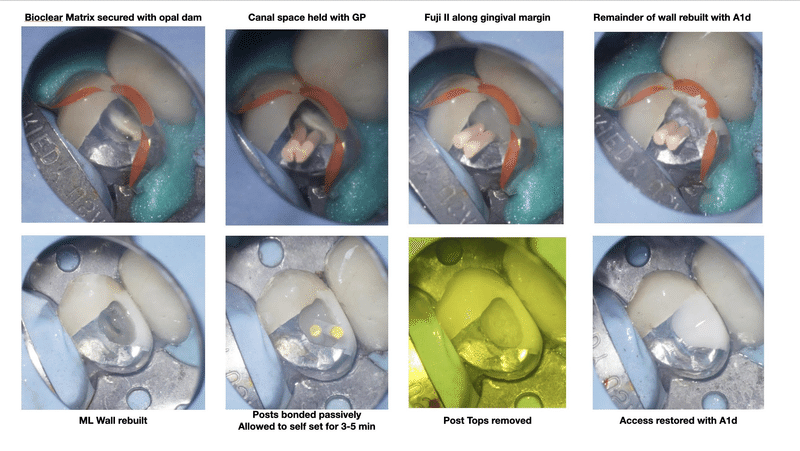


------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
top previous next 2. Re: Deep recurrent caries on 2-unit bridge... (dun dun dun sound effect)
Nicely-done under very challenging conditions with a tremendous amount of decay extending to the osseous level...at least! I'm curious if you ground off the porcelain on the distal marginal ridge, or if it chipped off during your access. In either case, what strategy did you use to have confidence that your composite reconstruction of the DMR would not snap off under function?
------------------------------
C. John Munce
Diplomate American Board of Endodontics
Sandpoint Idaho
(805)570-8666
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 11-28-2023 07:43 AM
From: Brent M. Hiebert
Subject: Deep recurrent caries on 2-unit bridge... (dun dun dun sound effect)
Below is a case I treated last week.
77 y/o male with deep recurrent mesial caries on tooth 12. Teeth 12 and 13 are a 2-unit bridge. The patient wanted to retain the bridge if possible and the referring dentist gave no information or guidance for the case. So this is what we did:
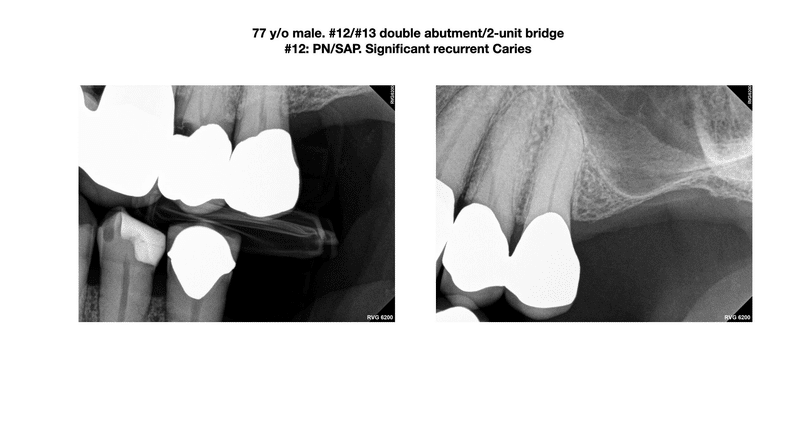



------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
top previous next 3. Re: Stella Life Promotional video

------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 11-20-2023 08:06 AM
From: A.K. Bobby Mallik
Subject: Stella Life Promotional video
Really disappointed to see the recent promotional video by stella life (stellalifehealing on instagram and im sure they are on other media outlets) where they interview a doc who openly speaks about "Should we do root canal treatments".
I want to respond to the post but need to calm down before i do.
Sincerely
Bobby Mallik
------------------------------
A. K. Bobby Mallik D. M. D
Diplomate, American Board of Endodontics
Durham NC
------------------------------
top previous 4. Re: Stella Life Promotional video

------------------------------
Douglas Robertson D.D.S.,M.S.
Wheeling WV
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate -------------------------------------------
Original Message:
Sent: 11-29-2023 07:34 AM
From: Brent M. Hiebert
Subject: Stella Life Promotional video
Bobby,
Just checking in to see how you are doing emotionally and if you have yet to calm down....
-----------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
You are subscribed to "AAE Discussion Open Forum" as toho_dental_club@yahoo.co.jp. Getting to many emails? Adjust your Community Notifications to the Weekly Digest option. To unsubscribe from this community discussion, go to Unsubscribe.
**********************************************************************************
--------------------------------------------------------------------
AAE24 Registration Opens Wednesday, December 6!
AAE24 #0A Save the DateYour VIP Pass to Education & Innovation If you are unable to see this message, click to view the web version.
Visit the AAE24 event listing and select "Download to Your Calendar" to save the date!
AAE24
APRIL 17-20,2024
LOS ANGELES
https://www.aae.org/specialty/wp-content/uploads/sites/2/2023/10/AAE24_SponsorshipProspectus_v3.pdf
*********************************************************************************
Post New Message Nov 23, 2023 Discussions
started one month ago, Brent M. Hiebert (38 replies) "Dueling" Cracked Teeth
1. Tooth 18: Previously initiated/SAP. A distal... Brent M. Hiebert

1. Re: "Dueling" Cracked Teeth Reply via Email Direct Reply to Sender
Nov 23, 2023 9:52 AM Brent M. Hiebert Tooth 18:
Previously initiated/SAP. A distal crack was noted during treatment 😥.
Following obturation, I extended my dual-cure composite deeeep down the distal canal and up through the access. The tooth was taken out of occlusion and will need to be crowned ASAP.
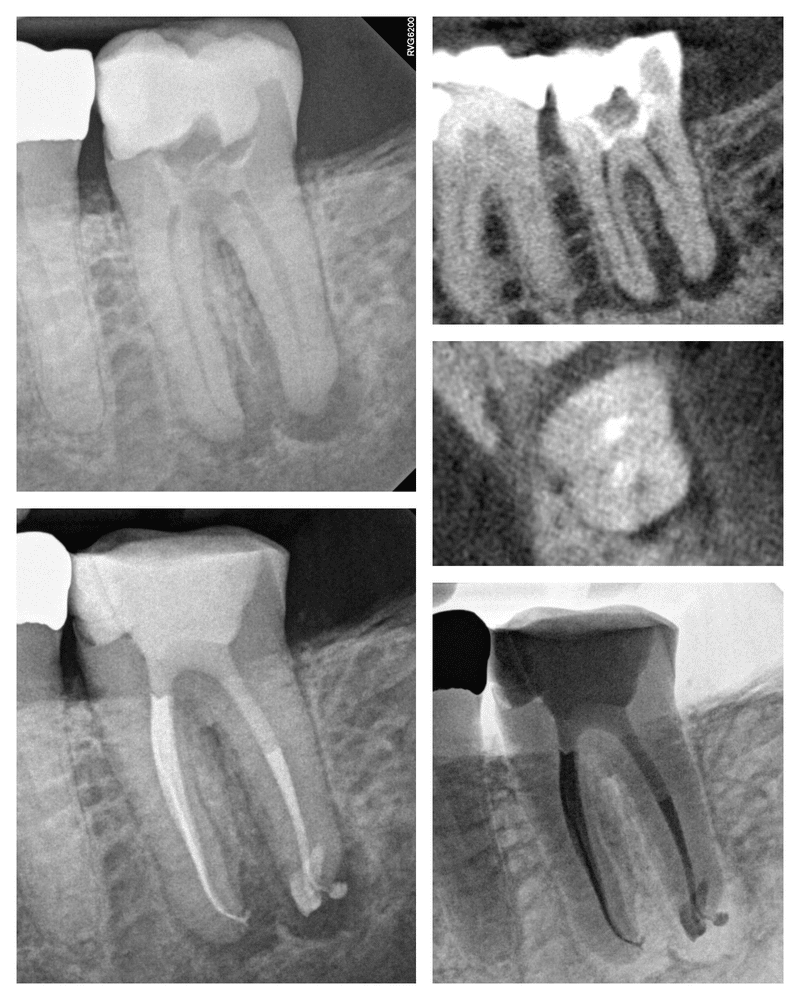
------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate
Original Message:
Sent: 11-16-2023 07:23 AM
From: Brent M. Hiebert
Subject: "Dueling" Cracked Teeth
Here's a case I treated Monday. SIP/SAP. My new Carestream 8200 died abruptly last week 🫨😰🥲(it's very uncomfortable working without one), so I did not have access to a scan but I expected cracks. No deep probings clinically. We moved forward with exploratory RCT. As expected, I noted a mesial and distal crack extending to pulp chamber. I prepped the cracks with ultrasonics and extended my restorative material deep down the canals.
Thankfully, my CBCT machine is now up and running


------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
You are subscribed to "AAE Discussion Open Forum" as toho_dental_club@yahoo.co.jp. Getting to many emails? Adjust your Community
Notifications to the Weekly Digest option. To unsubscribe from this community discussion, go to Unsubscribe.
*********************************************************************************
Post New Message Nov 21, 2023 Discussions
started 15 hours ago, Katherine Fry Hidi (0 replies) #30 pulpal necrosis with history of AAA on a 7 yr old girl 1. Thought I would share a special one with you... Katherine Fry Hidi started 6 months ago, Brent M. Hiebert (7 replies) 15/03 Preps 2. Thought I'd do a little CPR on this thread. ... Douglas N. Robertson 3. Doug, So I am using the 15/03 and 15/05... Brent M. Hiebert 4. Great, thanks. I wouldn't decrease my apical... Douglas N. Robertson top next 1. #30 pulpal necrosis with history of AAA on a 7 yr old girl Reply via Email Direct Reply to Sender

Nov 21, 2023 3:52 PM
view attached Katherine Fry Hidi Thought I would share a special one with you before the Thanksgiving holiday. Mostly, I'd love some insight on any treatment recommendations. I'm concerned about the success and prognosis of any treatment.
Patient was referred due to facial swelling that she has been treating with antibiotics. Per mom, the tooth showed signs of hypomineralized enamel even before it had erupted. Her pediatric dentist placed the filling back in July and wasn't in the office to speak with me today. Images don't look good. Wide open apices, widened PDL noted in all planes. Even if regenerative endodontics was initiated, has anyone applied it to a multi-rooted tooth? I'm concerned that the short root trunk will act like a perio-endo problem and compromise any treatment we try to perform, even if it is meant only to buy us time until #31 is ready to take its place. Thanks for your thoughts and recommendations!
------------------------------
Katie Fry Hidi D.M.D.
Atlanta GA
------------------------------
*********************************************************************************
Post New Message Nov 24, 2023 Discussions
started 23 hours ago, Brent M. Hiebert (0 replies) Laser Case. "Squirt" technique implemented for MB1
1. Laser-assisted RCT. I picked up some nice... Brent M. Hiebert started 2 days ago, Cami E. Ferris-Wong (3 replies) Do you believe in miracles?
2. I believe in miracles. Did you happen to... Brent M. Hiebert
3. Brent, I didn't take any photos, but now... Cami E. Ferris-Wong

top next 1. Laser Case. "Squirt" technique implemented for MB1 Reply via Email Direct Reply to Sender Nov 24, 2023 7:50 AMBrent M. Hiebert Laser-assisted RCT. I picked up some nice secondary anatomy within the MB root. I was not able to negotiate a GP cone to length, so I ended up needing to "squirt" the MB1 canal. For squirting, I injected the BC sealer hi flow (no disclosures) using a 29 gauge Navi tip (with a decent amount of pressure). I was able to get hand files to length, so I "shepherded" some of the sealer to length with a 10 c file. I injected more sealer and then injected warm GP into the canal and then applied firm pressure (down pack) to the warm GP with a plugger. During my last laser activation of my irrigants I probably extended my laser tip too far apically (single tear), started firing too quickly and ledged the canal. This likely led to my inability to place a GP cone. So far in the past two years ledging has rarely happened, but it is certainly a possibility when using the laser if one is forceful with the tip, trigger happy or on crazy pills (I can only imagine if @Douglas N. Robertson had a laser.... )

------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate

-------- Chase Thompson D.M.D. ------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate ----
Original Message:
Sent: 11-05-2023 07:53 AM
From: Brent Hiebert
Subject: "Dueling" Cracked Teeth
Another cracked tooth case I treated last week. No deep probings clinically, no obvious signs of a crack on CBCT imaging, however, this tooth had a large occlusal amalgam acting as a giant wedge ready to blast the tooth apart. Clinically, there was a crack on the mesial marginal ridge. I removed the amalgam and accessed the tooth. The crack was noted to extend roughly to where the pulp chamber started. I prepped the crack with ultrasonics and carried out RCT. A laser was used to help with cleaning and disinfection. The access was restored with a dual-cure material and the tooth was taken out of occlusion.

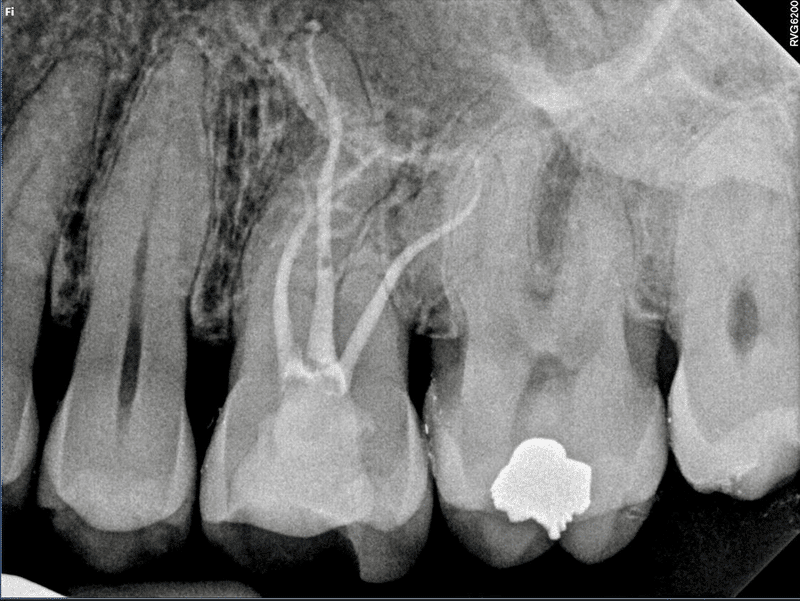
-----------------------------------------------------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics

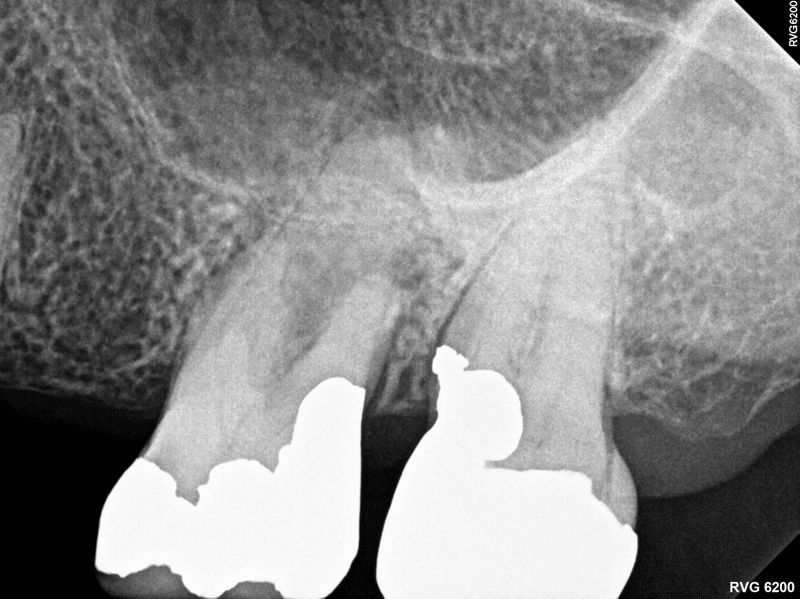



Oct 20, 2023 Discussions
started 19 hours ago, Brent M. Hiebert (0 replies) Deep Caries. Laser "Enhanced" RCT

1. Deep Caries. Laser "Enhanced" RCT Oct 20, 2023 11:22 AM Brent M. Hiebert @Omar Gabr here's an example of what I was talking about. The caries is in a different location than your case, but same general concept.
Tooth 18: SIP/SAP.
Place dental dam. Clamp tooth apical to tooth structure, typically directly on gingiva.
Laser away the excess tissue (gingivectomy)
Remove caries and old restoration
Rebuild wall (buccal wall in this case). I held the canal space with GP points and then free-flowed Fuji II glass ionomer and then smoothed it up
Isolate further with Flowable dam
Carry on with RCT
Blast the inside of the tooth with the laser, activate the Hypo etc
Obturate, taking precautions not to blast sealer into the mandibular canal
Restore the access
Check occlusion
Carry on with life
If you don't have a laser, a system b tip or diamond bur can be used for the gingivectomy.

------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate
You are subscribed to "AAE Discussion Open Forum" as toho_dental_club@yahoo.co.jp. Getting to many emails? Adjust your Community
Notifications to the Weekly Digest option. To unsubscribe from this community discussion, go to Unsubscribe.

I treated this case in a single visit. I used a laser for assistance with cleaning, disinfection, etc. I had the patient back yesterday for a 6 month followup check. Very nice apical healing was observed radiographically and the patient was asymptomatic.


レーザーの洗浄と消毒による

Nov 4, 2023 Discussions
started 15 hours ago, Brent M. Hiebert (0 replies) Single visit laser-assisted RCT. 6 month followup shows nice apical healing.
1. Single visit RCT with laser-assistance for... Brent M. Hiebert

1. Single visit laser-assisted RCT. 6 month followup shows nice apical healing. Reply via Email Direct Reply to Sender Nov 4, 2023 4:56 PM Brent M. Hiebert Single visit RCT with laser-assistance for cleaning and disinfection. 6 month followup shows nice apical healing.
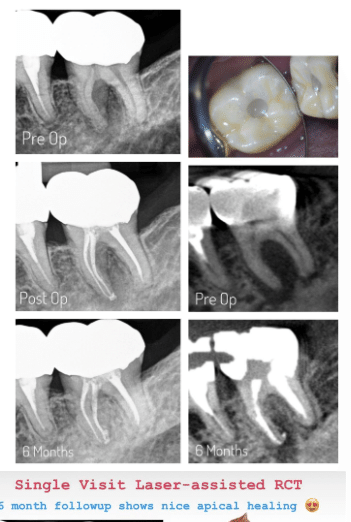

------------------------------
Brent M. Hiebert, DDS, MSD
Diplomate, American Board of Endodontics
Yamhill Valley Endodontic Specialists
McMinnville/Newberg, OR
IG: @hiebert.endodontics
------------------------------
Reply via Community View Thread Recommend Flag as Inappropriate
You are subscribed to "AAE Discussion Open Forum" as toho_dental_club@yahoo.co.jp. Getting to many emails? Adjust your Community Notifications to the Weekly Digest option. To unsubscribe from this community discussion, go to Unsubscribe.
この記事が気に入ったらサポートをしてみませんか?
