Problems and prospects in TMB-based cancer genomic medicine in Japan
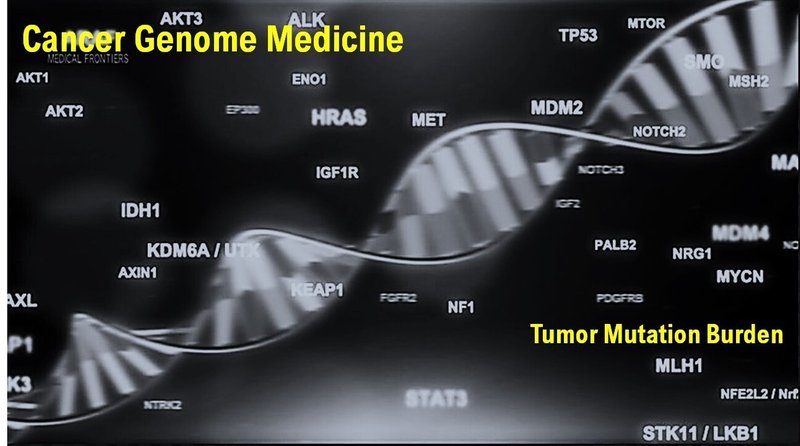
In addition to PD-L1 expression, various clinical factors are currently being investigated as predictors of the effectiveness of immune checkpoint inhibition. Tumor gene mutation burden (TMB) is the approximate amount of gene mutation that occurs in the genome of a cancer cell.
Originally, in mammalian cells including humans, a "gene repair system" that removes gene mutations is provided. However, cells with many TMBs have abnormalities in this repair system and are thought to be easily transformed into cancer cells (1,2).
In addition, cancer cells with many TMBs are thought to produce many mutant proteins that are recognized as foreign products by the self-immune system (3). Therefore, TMB has been established as an independent predictive biomarker for immune checkpoint inhibitors.
In the cases of tumor gene mutation burden-high (TMB-High), it has been observed high anti-tumor effect by immune checkpoint inhibitors (4,5).
On June 17, 2020, the US Food and Drug Administration (FDA) approved pembrolizumab (product name: Keytruda) monotherapy for unresectable or metastatic solid tumors with tumor gene mutation burden-high (TMB-High). In addition, on June 26, 2020, the FDA approved Foundation One CDx (Foundation Medicine, Inc.) as a companion diagnostic for pembrolizumab.
According to the guidelines of the Japanese Ministry of Health, Labor and Welfare, immune checkpoint inhibitors such as Nivolumab, Atezolizumab, and Pembrolizumab are recommended for patients with TMB-High (cutoff value of 10 or higher) from the results of the cancer genome test by NCC Oncopanel or Fundation One CDx, which are covered by insurance as a cancer genome test.
In Japan, medical treatments (total 576 cases) by cancer genome test (129 cases by NCC Oncopanel, 447 cases by Fundation One CDx) were performed at a national university hospital in 2020. Six of the 129 cases by NCC Oncopanel were diagnosed with TMB-High. However, close examination of the results of the cancer genome test revealed that 3 cases were erroneously diagnosed as TMB-High due to contamination of the sample. Of the 447 cases with Fundation One CDx, 19 were diagnosed with TMB-High. Only 4 cases were diagnosed with TMB-High 20 or higher.
Japan Ministry of Health, Labor and Welfare of has stated the following points as future issues.
1. In TMB, 10/MB is the cutoff value. However, is this 10/MB appropriate as a cutoff value to judge as TMB-High?
2. As a problem of quality control of samples, there is a concern about DNA fragmentation due to long-term storage of samples. As a problem with the sample collection site, there is concern about DNA fragmentation due to radiation therapy (RT).
Many patients with advanced refractory cancer with MSI-High are given the option of being treated with immunotherapy. It is important to improve the problems that have been recognized in the conventional cancer genome testing and medical treatment. In the future, if it becomes cheaper and the need for tissue collection and pathological tissue becomes less, the cancer genome test is likely to be more accessible for many cancer patients.
Disclosure of potential conflicts of interest
The authors declare no potential conflicts of interest.
Acknowledgments
We thank all the medical staffs and co-medical staffs for providing and helping medical research at National Hospital Organization Kyoto Medical Center. We appreciate Crimson Interactive Japan Co., Ltd. for revising and polishing our manuscript by Native English.
References
1. Chalmers, Z.R. et al.: Analysis of 100,000 human cancer genomes reveals the landscape of tumor mutational burden. Genome Med. 9(1): 34, 2017.
2. Campbell, B.B. et al.: Comprehensive Analysis of Hypermutation in Human Cancer. Cell. 171(5): 1042-1056, 2017.
3. Galuppini, F. et al.: Tumor mutation burden: from comprehensive mutational screening to the clinic. Cancer Cell Int. 19: 209, 2019.
4. Rizvi H et al., Molecular determinants of response to anti-programmed cell death (PD)-1 and anti-programmed death-ligand 1 (PD-L1) blockade in patients with non-small-cell lung cancer profiled with targeted next-generation sequencing. J Clin Oncol 2018; 36(7): 633-641
5. Hellmann M et al., Nivolumab plus ipilimumab in lung cancer with a high tumor mutational burden. N Engl J Med 2018; 378(22): 2093-2104 JAMA Oncology Published on December 18 2020 by Kyoto@Takuma H
この記事が気に入ったらサポートをしてみませんか?
